What is Telemedicine and How Can I Get the Most from it?

by Ted Kyle, RPH, MBA; and Craig Primack, MD, FACP, FAAP, FOMA
Fall 2020
We are all coping with a lot of changes because of the COVID-19 pandemic. You may even be experiencing challenges with seeing medical professionals in their offices since the current healthcare landscape looks very different right now. Because of this, more and more providers are using telemedicine to meet with patients for routine visits.
What is Telemedicine?
Telemedicine is an opportunity to visit with your healthcare provider or a medical professional through video conferencing or phone instead of an in-person office visit. Depending on the reason for your visit, medical professionals can offer advice, do check-ups or prescribe you with medication to treat any illnesses or symptoms you may be experiencing.
Some of the medical professionals you can connect with include:
- Physicians
- Surgeons
- Nurse practitioners
- Dietitians
- Physician assistants
- Mental health counselors
Face-to-face Telemedicine
During your face-to-face telemedicine visit, you can talk with your provider in real-time using phone or video chat. They can ask you questions and you can describe how you’re feeling, much like you would do in a regular office visit. Common platforms used for telemedicine video chats include:
- FaceTime
- Zoom
- Google Duo
- Skype
For telemedicine visits performed using video chats, you will typically need an internet-connected device that has a camera and microphone. This can be as simple as using any smartphone, mobile device, desktop or laptop computer.
Although appointments done via video chat may not be as personal as in-office visits, you can still see your provider and they can see you. However, while face-to-face telemedicine is a simple solution, especially in times like these, it is not HIPAA compliant. This means that while medical professionals and patients can use video chat to communicate, there is always a chance someone else could hear your private medical information.
Telemedicine through Messaging
The other option you have through telemedicine is the ability to communicate with your provider using text messaging, virtual text chats or email. The flexibility of these options lets you send a message anytime you want so you don’t have to wait until both of you are available. Your message might be a recorded video, voice message or even a text message – and your provider can retrieve it later and respond as soon as they are able to. Ideally, this option for telemedicine will use a system that’s designed to protect your medical privacy.
Benefits of Telemedicine
There are two major benefits that come with using telemedicine:
Saving Time: Patients spend an average of two hours for a 20-minute in-person office visit, including travel and wait time. Telemedicine can give you options for visits right when you need them. Spending less time in a waiting room can also decrease your chances of possibly contracting an illness. Before COVID-19, telemedicine was used primarily for rural and specialty consultations because it saved so much travel and wait time. But now, due to COVID-19, telemedicine visits have increased because patients can see their providers and still protect their health by social distancing.
Saving Money: Telemedicine also saves money, which makes it very convenient. It will usually eliminate the need to take time off work, drive anywhere, or find help for taking care of a child or elder for the duration of the appointment. A telemedicine visit can also be less expensive, or have no cost at all, depending on what insurance carrier you have.
Limitations of Telemedicine
Of course, there are also limitations to a telemedicine visit. These visits are usually best for routine medical appointments, surgical follow-up visits or minor illnesses. In a telemedicine visit, your provider cannot perform a physical exam that might be needed for a complete diagnosis. They might need to see you in-person to decide on the need for further testing. In addition, a good physical exam can help diagnose or narrow down medical conditions that are hard to diagnose over the phone or in a video chat.
Common Conditions a Primary Care Provider May Treat Using Telemedicine:
- Allergies
- Asthma
- Cold and flu
- Diarrhea
- Infections
- Insect bites
- Rashes
- Respiratory infections
- Skin inflammations
- Sore throats
- Bladder infections
- UTIs
- Vomiting
- Sport injuries
Telemedicine and Weight
If your telemedicine visit is specifically about your weight, weight loss or weight-related health conditions, it helps for you to have a home scale and a blood pressure device. You’ll want to take measurements before you start your visit so you can share them with your healthcare provider. They will want to have this data when the visit begins.
Specifically, if you want a healthcare provider to help you manage your weight, you will want to work with a medical professional who understands the challenges. A good resource to help you find a qualified obesity care provider is the Obesity Action Coalition’s Provider Locator at ObesityCareProviders.com. This resource offers a searchable and comprehensive list of healthcare providers with experience in treating obesity.
Some of the healthcare providers you can find through telemedicine include:
- Obesity medicine physicians
- Registered dietitian nutritionists
- Nurse practitioners
- Bariatric surgeons
- Psychologists
If you have struggled with losing weight in the past, it may help to begin with an ABOM-certified physician. ABOM stands for the American Board of Obesity Medicine. Certification as an ABOM diplomat means that a healthcare provider has specialized knowledge in obesity medicine. This certification distinguishes a physician as having achieved expertise in obesity care. Physicians and bariatric surgeons may hold this designation.
Telemedicine Apps/Software:
- Doxy.me
- AMC Health
- Teladoc
- swyMed
- Mend
- MDLIVE
- LiveHealth
- PlushCare
- Doctors on Demand
- Express Care Virtual
Conclusion
Telemedicine is a great way to meet with a healthcare provider while saving time, money, and avoiding possible illnesses. All of these benefits are especially important to have during times like these. If telemedicine is an option for you and you have access to the appropriate devices, apps or software, try it out! It could save you an extra trip to the doctor’s office.
About the Authors:
Ted Kyle, RPh, MBA, founded his blog, ConscienHealth, in 2009. He is a pharmacist and healthcare innovation professional who works with health and obesity experts for sound policy and innovation to address obesity. Mr. Kyle serves on the Board of Directors for the Obesity Action Coalition (OAC), advises The Obesity Society (TOS) on advocacy issues and consults with organizations addressing the needs of people living with obesity. His widely-read daily commentary, published at ConscienHealth.org, reaches an audience of more than 10,000 thought leaders in health and obesity.
Craig Primack, MD, DACP, FAAP, FOMA, is certified in obesity medicine and has been practicing full time medical weight management since 2006. He is currently the president of the Obesity Medicine Association (OMA) and co-author of “Chasing Diets,” a book about the science of medical weight loss published in 2019. Find out more about Dr. Primack and watch his video blog at DoctorPrimack.com.
Considering a robotic surgery procedure? In this Health Talk, you’ll hear from bariatric surgeon Walter Medlin, MD,…
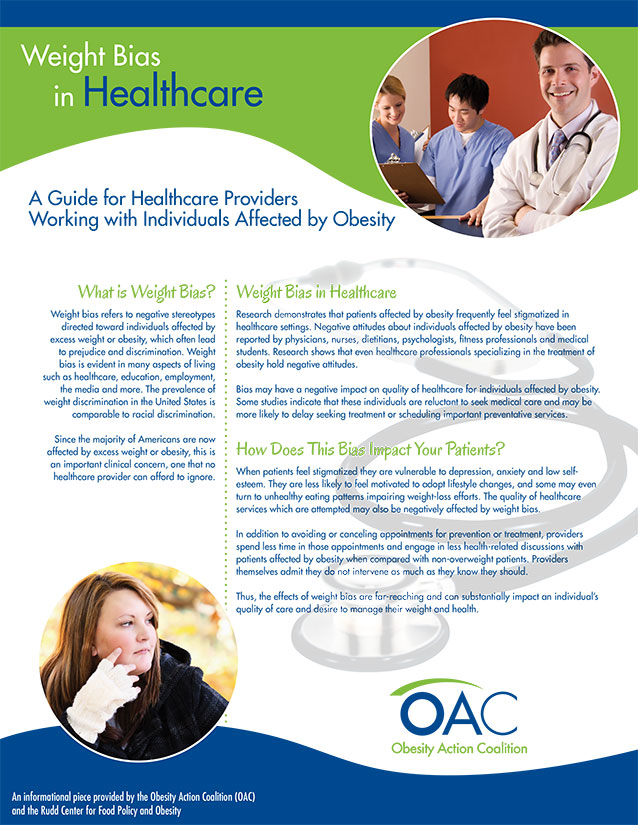
View VideoThe focus of this guide is to educate healthcare providers on the impact of weight bias in…
View GuideThe OAC would like to thank the Rudd Center for Food Policy and Obesity for assistance in…
Download Brochure