Understanding Obesity Stigma Brochure

The OAC would like to thank the Rudd Center for Food Policy and Obesity for assistance in creating this brochure.
“The alarming rates of obesity have brought widespread attention to the medical consequences of this public health problem. Often ignored, however, are the social and personal obstacles that individuals with excess weight or obesity face. Bias, stigma, and discrimination due to weight are frequent experiences for many individuals with obesity, which have serious consequences for their personal and social well being and overall health. Given that at least half of the American population is overweight, the number of people potentially faced with discrimination and stigmatization is immense.”
– Rebecca Puhl, PhD, Deputy Director at the Rudd Center for Food Policy and Obesity at the University of Connecticut.
Weight stigma plays a role in everyday life, including work, school and healthcare settings. It remains a socially acceptable form of prejudice in American society, and is rarely challenged. One of the goals of the Obesity Action Coalition (OAC) is to eliminate the negative stigma associated with obesity. To do this, we must be able to define and recognize obesity stigma in all aspects of life. Once we are able to identify the nature and extent of this problem, we can increase education and awareness about the damaging and lasting effects of negative stigma.
Throughout this brochure, we will discuss the many forms of stigma and provide readers with options for dealing with stigma and ways to educate others.
Causes of Obesity:
Perceptions May Perpetuate Negative Stigma
Perceptions about the causes of obesity may contribute to weight stigma and bias. Assumptions that obesity can be prevented by self-control, that individual non-compliance explains failure at weight-loss, and that obesity is caused by emotional problems, are all examples of attitudes that contribute to negative bias.
Research suggests that beliefs about the causality and stability of obesity are also important factors contributing to negative attitudes. For example, studies show that individuals affected by obesity are more likely to be stigmatized if their overweight condition is perceived to be caused by controllable factors compared to uncontrollable factors (e.g., overeating versus a thyroid condition), and if obesity is perceived to be a condition of personal choice, versus a serious health condition.
Bias in Employment Settings
At Work
There is clear evidence of weight stigma and bias in multiple aspects of daily life for individuals affected by obesity. Negative perceptions of people affected by obesity exist in employment settings where employees affected by obesity are viewed as less competent, lazy and lacking in self discipline by their co-workers and employers. These attitudes can have a negative impact on wages, promotions and decisions about employment status for employees affected
by obesity.
Experimental studies also show that applicants affected by obesity are less likely to be hired than thinner applicants, despite having identical job qualifications. There are also increasing legal cases emerging where employees affected by obesity have been fired or suspended because of their weight, despite demonstrating good job performance and even though their body weight was unrelated to their job responsibilities.
Bias in employment settings has been identified in the following areas:
- Hiring preferences
- Promotions
- Wage inequities
- Employment termination
Hiring Preferences:
Job applicants affected by obesity are rated as having:
- Poor self-discipline
- Low supervisory potential
- Poor personal hygiene
- Less ambition & productivity
- Higher likelihood of being hired for a job requiring little face-to-face contact
Promotions:
Applicants affected by obesity are rated as having:
- Lower promotion prospects compared to non-overweight counterparts
- Harder time being recommended by managers for promotion, as compared to other candidates
- Less of a chance to get hired in high-level positions
Wage Inequities:
The following are true in regards to wage inequities for individuals affected by obesity:
- Women affected by obesity earn as much as 12 percent less than females not affected by obesity.
- Women affected by obesity are more likely to be in low-paying jobs than thinner women.
- Men affected by obesity are under-represented and are paid less than men not affected by obesity in managerial and professional positions.
Employment Termination:
Employees affected by obesity are affected more often in the following examples than employees not affected by obesity:
- Fired due to prejudiced employers and arbitrary weight standards
- Fired despite good to excellent employment records for occupations such as: teachers, pilots, office managers, state troopers and city laborers
Bias in Education
In School
Multiple forms of weight stigmatization also occur in educational settings. Students affected by obesity face numerous obstacles, ranging from harassment and rejection from peers at school, to biased attitudes from teachers, lower college acceptances and wrongful dismissals from college.
The severity of this problem is highlighted by research showing that stigma toward students affected by obesity begins very early. For example, negative attitudes have been reported among pre-school children (ages three to five) who associated peers affected by obesity with characteristics of being mean, stupid, ugly and having few friends.
Bias in education is expressed through extensive peer victimization at school, and negative attitudes by teachers, administrators and academic institutions.
Weight Bias by Peers:
- Negative attitudes begin as early as preschool.
- Children affected by obesity are teased by kids and chosen less as playmates.
- Stigmatization continues through high school and college, where students affected by obesity are viewed as self-indulgent, lazy and are excluded from social activities.
Peer Victimization:
- At least 30 percent of girls with excess weight and 24 percent of boys with excess weight report being teased by peers at school.
- Adolescents at the heaviest weight are most likely to be teased because of their weight.
- Overall, as many as 63 percent of girls and 58 percent of boys report peer victimization.
- Having excess weight predicts future peer victimization.
Bias by Educators:
- Teachers report that students affected by obesity are perceived as:
- Untidy
- More emotional
- Less likely to succeed at school
- More likely to have family problems
Educational Institutions:
- Children with excess weight are less likely to be accepted to college, despite equivalent application rates and academic achievement.
- Students affected by obesity are sometimes dismissed from college because of their weight.
Weight Bias in Healthcare
In Healthcare Settings
Unfortunately, weight stigma also exists in healthcare settings. Negative attitudes about individuals with excess weight have been reported by physicians, nurses, dietitians, psychologists and medical students. Research shows that even healthcare professionals who specialize in the treatment of obesity hold negative attitudes.
Bias may have a negative impact on quality of healthcare for individuals affected by obesity. Some studies have indicated that these individuals are reluctant to seek medical care, and may be more likely to delay important preventative healthcare services and cancel medical appointments. Weight bias has been reported as one reason for these negative experiences.
Research indicates that 46 percent of women affected by obesity reported that small gowns, narrow exam tables and inappropriately sized medical equipment were barriers to receiving healthcare. In addition, 35 percent reported embarrassment about being weighed as a barrier to care.
(source: Amy NK, Aalborg A, Lyons P, & Keranen L. Barriers to routine gynecological cancer screening for White and African-American women with obesity. Int J Obesity & Related Metabolic Disorders. 2006; 30: 147-155.)
Physicians:
Self-report studies show that physicians often view individuals affected by obesity as described below more often than they do individuals not affected by obesity :
- Non-compliant
- Dishonest
- Lazy
- Lacking in self-control
- Weak-willed
- Unintelligent
- Unsuccessful
Physicians are common sources of stigma. In a study that surveyed more than 2,400 adult women about their experiences of weight bias, 69 percent of respondents reported that physicians were a source of weight bias, and 52 percent reported they had been stigmatized by a doctor on multiple occasions.
Doctors were the second most frequent source of bias reported, out of a list of more than 20 possible sources of weight stigma.
(source: Puhl, R., & Brownell, K.D. (2006). Confronting and coping with weight stigma: An investigation of overweight and individuals with obesity. Obesity, 14, 1802-1815.)
Nurses:
Self-report studies show that nurses view individuals affected by obesity as non-compliant, overindulgent, lazy and unsuccessful. Studies of self-reported attitudes among nurses indicate that:
- 31 percent “would prefer not to care for individuals affected by obesity”
- 24 percent agreed that individuals affected by obesity “repulsed them”
- 12 percent “would prefer not to touch individuals affected by obesity”
Psychologists:
In studies comparing beliefs about individuals affected by obesity versus “average” weight individuals, psychologists ascribe the following attributes to clients affected by obesity:
- More pathology
- More severe psychological symptoms
- More negative attributes
- Worse prognosis in treatment
Quality of Care:
- Individuals affected by obesity are also more likely to have the following challenges with quality of care:
- Fewer preventive health services and exams
- Less access to cancer screening tests, such as pelvic exams and mammograms
- More frequent cancellation or delay of appointments
- Less time spent with the physician, less intervention and less discussion with the physician
Consequences of Weight Bias
Taken together, the consequences of being denied jobs, rejected by peers and treated inappropriately by healthcare professionals because of one’s weight can have a serious and negative impact on quality of life. Individuals affected by obesity suffer terribly from this, both from direct discrimination and from more subtle forms of bias that are frequently encountered.
Weight bias can have psychological, social and physical health consequences on those affected by this disease.
Psychological outcomes can include:
- Depression
- Anxiety
- Low self-esteem
- Poor body image
The social effects can include:
- Social rejection by peers
- Poor quality of interpersonal relationships
- Potential negative impact on academic outcomes
The physical health outcomes can include:
- Unhealthy weight control practices
- Binge-eating
- Avoidance of physical activity
What Can Be Done to Eradicate the Problem of Weight Bias?
Given how acceptable weight stigma is in our society, transforming societal attitudes and enacting laws that prohibit discrimination based on weight are needed in order to eliminate the problem of stigma toward individuals affected by obesity. Although this requires enormous efforts, there are other important steps that can be taken by both individuals and their healthcare providers to help improve the daily functioning and well-being of individuals affected by obesity.
Individuals as Advocates
Individuals who are struggling with weight stigma can begin to approach this problem by becoming advocates for themselves. This includes identifying situations in which they have been stigmatized because of their weight and deciding how best to handle the situation to achieve positive emotional health and to help prevent additional stigma from occurring. Specific strategies for dealing with weight stigma are highlighted below.
Individual Strategies to Deal with Weight Stigma:
- Educate others about the stigma of obesity to help challenge negative attitudes.
- Obtain social support from others who are struggling with weight stigma, or from friends and family members who are supportive.
- Instead of avoiding enjoyable activities because of negative feelings about your weight, set goals to ease these restrictions and participate more fully in these experiences.
- Rather than feeling inferior, practice positive self-talk strategies that emphasize self-acceptance and positive self-esteem.
- Be vocal about individual needs and positively assert these to appropriate individuals (e.g., requesting larger-sized medical gowns from a healthcare provider).
- Communicate to the perpetrator of bias that his or her comments were inappropriate and hurtful, and that nobody deserves such unkind remarks, regardless of their weight.
- Talk to a therapist to help identify effective ways to cope with stigma and to replace self-defeating thoughts or self-blame with healthier ways of coping.
It is important to note that there are many different strategies of coping with weight stigma and some strategies may be more or less effective with different types of stigmatizing situations.
An Important Role for Healthcare Professionals
Healthcare can easily become a negative and shaming experience for individuals affected by obesity because of weight stigma. Therefore, healthcare professionals have an extremely important role to play in addressing the problem of weight bias.
Encouraging individuals to share their experiences of stigma and to help them feel less isolated in these experiences is an important first step. Clinicians can also help individuals identify ways to effectively cope with stigma, such as using positive “self-talk,” obtaining social support from others and participating in activities that they may have restricted due to feelings of shame about their weight.
These tools can help reduce the tendency of individuals affected by obesity to internalize negative stereotypes of obesity and blame themselves, both of which can negatively impact emotional well-being.
A second role for healthcare professionals is to address the issue of weight bias within themselves, their medical staff and colleagues. In order to be effective and empathic with individuals affected by obesity, this requires honest self-examination of one’s own attitudes and weight bias. Education can help increase awareness among healthcare professionals about the pervasiveness and consequences of weight bias and can also encourage providers to adopt a more accurate and empathic understanding of their patients affected by obesity.
Finally, healthcare professionals can do a great service to their patients affected by obesity by improving the physical and social environment of healthcare settings. This means having bathrooms that are easily negotiated by heavier individuals, sturdy armless chairs in waiting rooms, offices with large exam tables, gowns and blood pressure cuffs in appropriate sizes and reading materials for individuals that are appropriate and “weight-friendly” (rather than fashion magazines with thin supermodels). The following checklist provides suggested guidelines to improve the healthcare environment for individuals affected by obesity:
Exam Room
- Stepstool with handle for exam table access
- Large sized gowns
- Large and extra large adult and thigh blood pressure cuffs
- Long vaginal specula
- Wide examination tables, bolted to the floor
- Hydraulic tilt tables
- Sturdy armless chairs
Waiting Room
- Open arm chairs that can support more than 300 pounds
- Firm sofas that can support more than 300 pounds
- Ensure 6-8 inches of space between chairs
- Weight-sensitive reading materials
- Doors and hallways accommodating large size wheelchairs, walkers and scooters
- Bathrooms with split lavatory seat with handled urine specimen collector
- Bathrooms with properly mounted grab bars and floor-mounted toilets
Scale
- Wide-based scale that measures greater than 350 pounds
- Meets established accuracy requirements
- Accessible for individuals with disabilities
- Situated in a physical location that offers privacy and confidentiality
- Wide platform with handles for support during weighing
Healthcare professionals can also improve their interpersonal interactions by being sensitive to situations of embarrassment for individuals, such as weighing individuals in a private and sensitive manner, without judgmental commentary. Asking individuals for their permission to be weighed at each visit is an easy and sensitive way to begin the weighing procedure. Providers can also help by emphasizing goals of health and fitness behaviors (rather than only the number on the scale) and celebrating positive health behavior changes made by individuals.
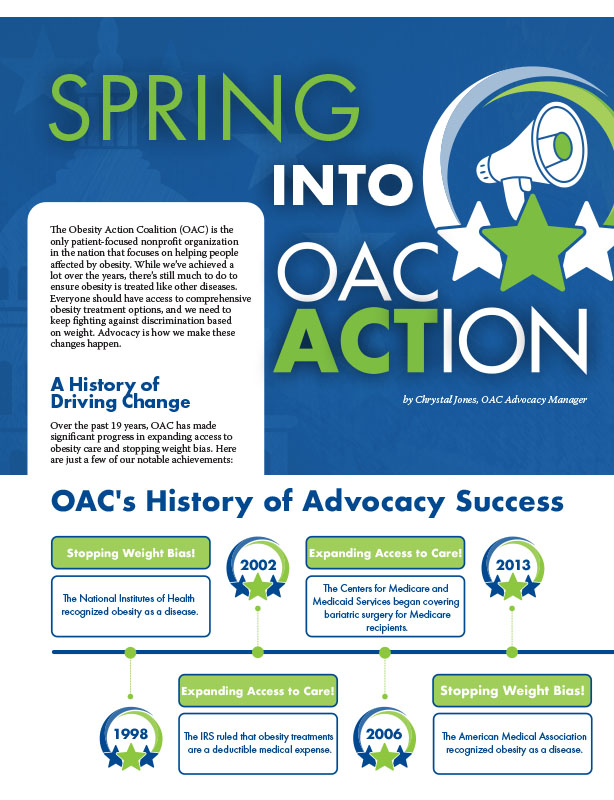
by Chrystal Jones, OAC Advocacy Manager Spring 2024 The Obesity Action Coalition (OAC) is the only patient-focused…
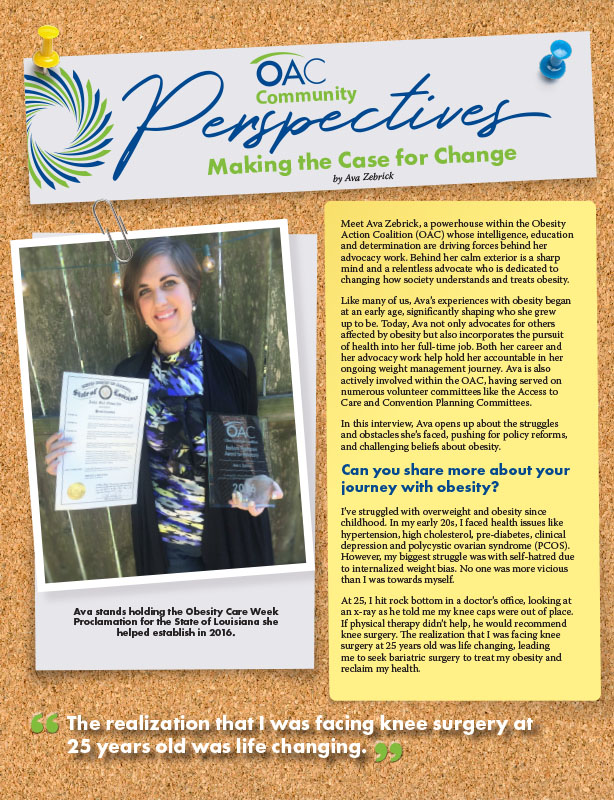
Read Articleby Ava Zebrick Spring 2024 Meet Ava Zebrick, a powerhouse within the Obesity Action Coalition (OAC) whose…
Read ArticleThe OAC is honored to welcome three new members to the OAC National Board of Directors. Jason Krynicki,…
Read Article