Weight-loss Surgery, Nutrition and Hair Loss

by Jacqueline Jacques, ND
Winter 2011
Typically, about 90 percent of hairs are anagen (in a growth phase) and 10 percent are telogen (in a dormant or resting phase) at any given time, meaning you are usually losing a lot less hair than you are growing so you don’t have noticeable hair loss. But sometimes this can change.
A common fear and complaint of bariatric surgery patients is post-operative hair loss. While for most of us as people, our hair is an important part of our self-image and body image, it is not very important to our bodies. For this reason, nutrition can have a great impact on hair health because when forced to make a choice, the body will shift nutritional stores to vital organs like your brain and heart and away from your hair.
Hair loss has many causes. The most common type of hair loss after weight-loss surgery is a diffuse loss known medically as telogen effluvium, which can have both nutritional and non-nutritional causes.
Growing and Losing Hair
Whether you are aware of it or not, for most of your life you are always in the process of both growing and losing hair. Human hair follicles have two states; anagen, a growth phase, and telogen, a dormant or resting phase. All hairs begin their life in the anagen phase, grow for some period of time, and then shift into the telogen phase which lasts for about 100 to 120 days. Following this, the hair will fall out.
Specific types of stress can result in a shift of a much greater percentage of hairs into the telogen phase. The stressors known to result in this shift, or telogen effluvium, include:
|
Weight-loss Surgery and Hair Loss
Nutritional issues aside, bariatric surgery patients already have two major risks of major surgery and rapid weight-loss. These alone are likely to account for much of the hair loss seen after surgery. In the absence of a nutritional issue, hair loss will continue until all hairs that have shifted into the telogen phase have fallen out. There is no way of switching them back to the anagen phase.
Hair loss rarely lasts for more than six months in the absence of a dietary cause. Because hair follicles are not damaged in telogen effluvium, hair should then regrow. For this reason, most doctors can assure their weight-loss surgery patients that with time and patience, and keeping up good nutritional intake, their hair will grow back. Discrete nutritional deficiencies are known to cause and contribute to telogen effluvium. One would be more suspicious of a nutritional contribution to post-bariatric surgery hair loss if:
|
Nutrition Iron
Iron is the single nutrient most highly correlated with hair loss. The correlation between non-anemic iron deficiency and hair loss was first described in the early 1960s, although little to no follow-up research was conducted until this decade. While new research is conflicted as to the significance of ferritin as a diagnostic tool in hair loss, it has still been found that a significant number of people with telogen effluvium respond to iron therapy.
Optimal iron levels for hair health have not been established, although there is some good evidence that a ferritin level below 40ug/L is highly associated with hair loss in women.1 It is worth noting that this is well above the level that is considered to be anemia, so doctors would not be expected to see this as a deficiency.
Zinc
Zinc deficiency has been tied to hair loss in both animal studies and human cases. There is data linking zinc deficiency in humans to both telogen effluvium and immune-mediated hair loss. Zinc deficiency is a well-recognized problem after bileopancreatic diversion/duodenal switch, and there is some indication that it may occur with other procedures such as gastric bypass and adjustable gastric banding.
In 1996, a group of researchers chose to study high dose zinc supplementation as a therapeutic agent for related hair loss2 in patients with vertical banded gastroplasty. The study administered 200 mg of zinc sulfate (45mg elemental zinc) three times daily to post-operative patients with hair loss. This was in addition to the multivitamin and iron supplements that patients were already taking. No labs for zinc or other nutrients were conducted.
Researchers found that in patients taking the zinc, 100 percent had cessation of hair loss after six months. They then stopped the zinc. In five patients, hair loss resumed after zinc was stopped, and was arrested again with renewed supplementation. It is important to note that in telogen effluvium of non-nutritional origin, hair loss would be expected to stop normally within six months. Since the researchers conducted no laboratory studies, and there was no control group, the only patients of interest here are those who began to lose hair again after stopping zinc. Thus we cannot say that zinc would prevent hair loss after weight-loss surgery, and further study would definitely be needed to make this connection.
A further note: The Tolerable Upper Intake Level (UL) for zinc is set at 40mg in adults. This study utilized a daily dose of more than three times that level. Not only can these levels cause gastrointestinal distress, but chronic toxicity (mostly associated with copper depletion) can start at levels of 60 mg/day. Information related to this study has made its way to many a support group and chat room – even to doctor’s offices – with the message of “high dose zinc will prevent hair loss after weight-loss surgery.” Patients should be advised that high dose zinc therapy is unproven and should only be done under supervision due to the associated risks of toxicity. A lab test to check for zinc deficiency would be best before giving a high dose such as this.
Protein
Low protein intake is associated with hair loss. Protein malnutrition has been reported with duodenal switch, and in gastric bypass to a much lesser degree. Little is known about incidence, as only around eight percent of surgeons track labs such as total protein, albumen or prealbumen. Limited studies suggest that patients with the most rapid or greatest amounts of weight-loss are at greatest risk.3
With surgical reduction of the stomach, hydrochloric acid,4 pepsinogen5 and normal churning are all significantly reduced or eliminated. Furthermore, pancreatic enzymes that would also aid in protein digestion are redirected to a lower part of the small intestine. It is thus likely that maldigestion, rather than malabsorption, is responsible for most cases. Some studies have also implicated low protein intake.6
Research also indicates that low levels of the amino acid l-lysine can contribute to hair loss and that repletion of lysine stores may both improve iron status and hair regrowth. In a study of anemic patients with hair loss who were supplemented with 1.5 to 2 grams of l-lysine in addition to their iron therapy, ferritin levels increased more substantially over iron therapy alone.1
Many individuals believe that supplementing with or topically applying the nutrient biotin will either help to prevent hair loss or will improve hair regrowth. To date, there is no science that would support either of these presumptions. While biotin deficiency can cause dermatitis, hair loss is only known to occur in experimentally induced states in animal models or in extreme cases of prolonged diets composed exclusively of egg whites.7
Other
Other nutrients associated with hair health include vitamin A, inositol, folate, B-6 and essential fatty acids. Hair loss can also be caused by systemic diseases, including thyroid disease and polycystic ovarian syndrome (PCOS) and is influenced by genetics.
Conclusion
Hair loss can be distressing to bariatric surgery patients and many will try nutrition themselves to see if they can prevent it. Unfortunately, there is little evidence that early hair loss is preventable because it is mostly likely caused by surgery and rapid weight-loss.
Later hair loss, however, can be indicative of a nutritional problem, especially iron deficiency, and may be a clinically useful sign. Educating patients about the potential for hair loss and possible underlying causes can help them to make informed choices and avoid wasting money on gimmicks that may have little real value.
About the Author:
Jacqueline Jacques, ND, is a Naturopathic Doctor with more than a decade of expertise in medical nutrition. She is the Chief Science Officer for Catalina Lifesciences LLC, a company dedicated to providing the best of nutritional care to weight-loss surgery patients. Her greatest love is empowering patients to better their own health. Dr. Jacques is a member of the OAC National Board of Directors.
References:
- Rushton DH. Clin Exp Dermatol. 2002 Jul;27(5):396-404.
- Neve H, Bhatti W, Soulsby C, Kincey J, Taylor T. Reversal of hair loss following vertical gastroplasty when treated with zinc sulphate. Obes Surg. 1996 Feb, 6(1):63-65.
- Updegraff TA, Neufeld NJ. Protein, iron, and folate status of patients prior to and following surgery for morbid obesity. J Am Diet Assoc. 1981;78(2):135–140
- Segal A, Kinoshita Kussunoki D, Larino MA. Postsurgical refusal to eat: anorexia nervosa, bulimia nervosa or a new eating disorder? A case series. Obes Surg. 2004;14(3):353–360.
- Behrns KE, Smith CD, Sarr MG. Prospective evaluation of gastric acid secretion and cobalamin absorption following gastric bypass for clinically severe obesity.
- Dig Dis Sci. 1994 Feb;39(2):315-20.
- Moize V, Geliebter A, Gluck ME, et al. Obese patients have inadequate protein intake related to protein intolerance up to 1 year following Roux-en-Y gastric bypass. Obes Surg. 2003;13(1):23–28.
- Mock DM. Biotin. In: Shils M, Olson JA, Shike M, Ross AC, eds. Nutrition in Health and Disease. 9th ed. Baltimore: Williams & Wilkins; 1999:459-466.
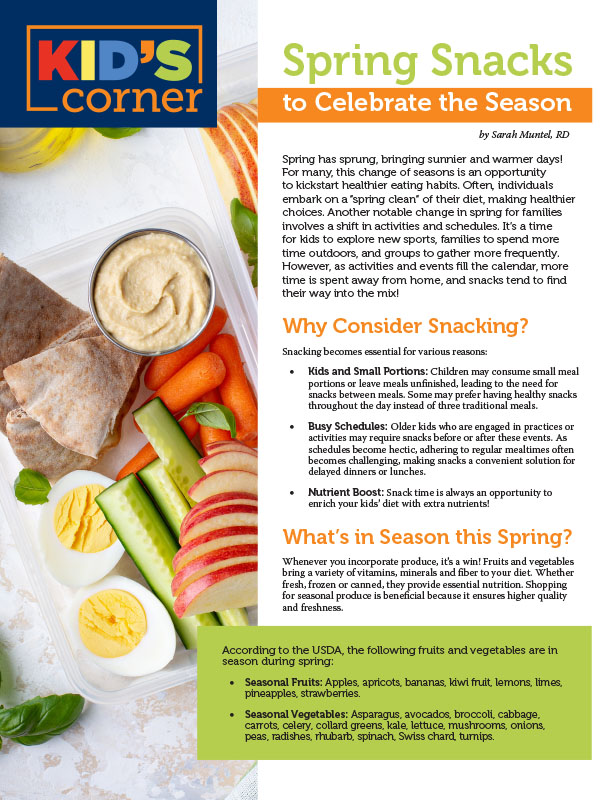
by Sarah Muntel, RD Spring 2024 Spring has sprung, bringing sunnier and warmer days! For many, this…
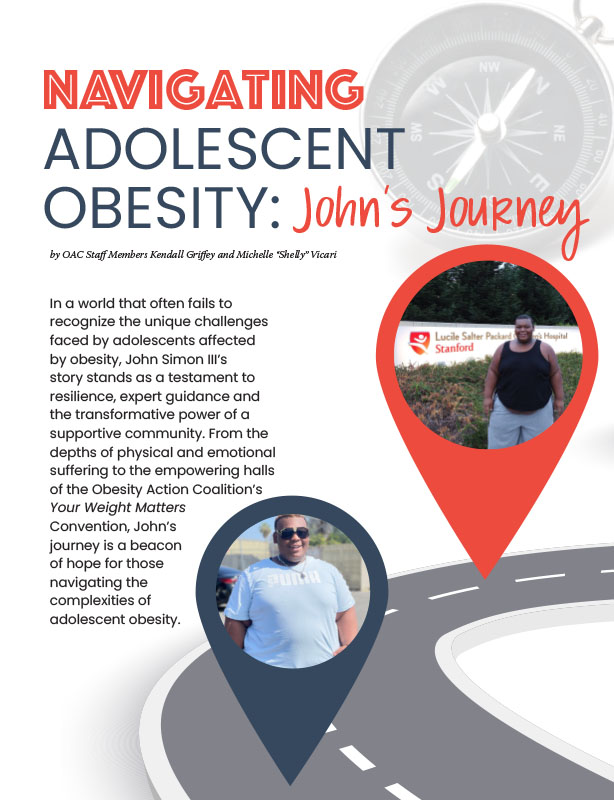
Read Articleby OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Article