Body Weight and Cancer: What You Need to Know


by Sarah Ro, MD; and Young Whang, MD, PhD
Fall 2023
Mary, a postmenopausal woman with a higher body weight and a BMI of 45, wanted to manage her weight by having bariatric surgery. The day before surgery, she had second thoughts and backed out. That was five years ago. Now, she is in the operating room, but it’s for a different kind of surgery. She’s having a mastectomy because she recently found out she had breast cancer.
Is There a Link Between Obesity and Cancer?
The link between obesity and cancer is clear. Having excess body fat increases the likelihood of developing various cancers, like breast, uterine, prostate, pancreatic, gallbladder, thyroid, colorectal, head and neck, and esophageal cancers. While not everyone carrying excess weight will necessarily develop cancer, their risk of getting cancer is higher.
Cancer is the second leading cause of death in the U.S. While there have been many important discoveries that lowered cancer rates, one thing stands out: cancers linked to obesity. These types of cancers make up about 40% of all cancer cases, which is about 684,000 annually.
The most prevalent obesity-related cancers are:
- Women: Postmenopausal breast cancer
- Men: Colorectal cancer
More than 90% of newly diagnosed obesity-related cancers are found in people aged 50 years and older. However, there is a growing trend of cancer among young people in the U.S. Experts believe that the rise in obesity among kids might be one reason for this increase.
What Factors Increase the Risk of Obesity-Related Cancers?
- Amount of Weight Gain: The risk of cancer associated with obesity is directly linked to the degree of weight gained. When individuals experience greater weight gain, their risk also increases.
- Duration of Excess Weight: The length of time a person carries excess weight significantly affects their risk of developing obesity-associated cancer. The longer someone carries extra weight, the greater their risk becomes.
- Weight Cycling: The pattern of repeatedly losing and regaining weight, commonly referred to as weight cycling, can raise the risk of obesity-associated cancer. This cycle of weight fluctuations might have adverse effects on the body’s systems.
- Impact of Childhood Obesity: Experiencing obesity during childhood has repercussions for cancer mortality rates in adulthood. Individuals who had obesity during their childhood are associated with a higher risk of mortality related to cancer during their adult years.
How Does Obesity Contribute to Cancer?
Experts have identified several ways that carrying excess body weight can elevate your risk of cancer. They include:
- Chronic Inflammation: Carrying extra body fat can lead to persistent, ongoing inflammation in the body. This makes the chance of getting cancer higher.
- Hormones: Fat cells in your body produce hormones, such as estrogen. Elevated estrogen levels from having excess fat can have a significant impact on breast cancer risk.
- Insulin and Growth Hormones: Excess body weight can lead to higher levels of insulin and insulin-like growth hormones, which have the potential to promote the development of cancer.
Importance of Cancer Screening
If you have obesity, it’s crucial to get the right cancer screening tests done at the recommended times. Please make an appointment with your healthcare provider for your annual checkup, where they will discuss cancer screening tests.
Challenges in Cancer Screening for People with Obesity
- Prostate Cancer Screening: Men with obesity might not show high levels of PSA in their blood. This makes it less likely for them to get a needle biopsy, which helps find prostate cancer. Because of this, prostate cancer might be found when it’s more advanced and harder to treat. Also, men with obesity tend to have higher mortality rates with prostate cancer. Some studies suggest that using an MRI test might help find prostate cancer in high-risk men with obesity, but it’s not always covered by insurance.
- Breast Cancer Screening: Women with obesity should request a special kind of mammogram called 3D mammography, if possible. This test can help find invasive breast cancer at a 40% higher rate than other screening tests. If your physician recommends an MRI for breast cancer screening because of your high risk or a gene mutation, be aware that some MRI machines might not support higher weights. Check this before you schedule the test.
- Colon Cancer Screening: Men with severe obesity (BMI over 40) have the lowest rate of colon cancer screening. Colon cancer is the top obesity-associated cancer among men with obesity. If you’re over 45 and have obesity, talk to your doctor about getting screened. Also, the rate of incomplete bowel preparation is much higher in patients with obesity, which could lead to missed polyps or cancers. Talk to your healthcare provider about how to prepare properly.
How Can I Reduce My Cancer Risk if I Am Overweight or Have Obesity?
Losing as little as 5-10% of your body weight can decrease your risk of cancer.
Strategies to Reduce Your Cancer Risk:
- Quit Smoking: If you smoke, talk to your doctor about how to stop. They can help you find resources to quit.
- Choose Water: Instead of sugary drinks like soda, juice, sweet tea and sports drinks, drink water. This can help you cut down on calories and lose weight.
- Limit Eating Out: Eating fast food or restaurant meals every day can sabotage your weight-loss efforts. Try preparing meals at home or packing your own food to eat. Frozen meals with protein and vegetables are good options, too.
- Avoid Crash Diets. Quick weight-loss diets don’t work well. Yo-yo dieting can lead to a cycle of losing and gaining weight, which increases your cancer risk.
- Stay Active: Find an activity you enjoy and do it regularly. Soon, it will become a habit. Research suggests that just three to four minutes of intense daily activity, like bursts of fast walking or stair climbing, can help lower your cancer risk.
- Talk About Medications: Ask your doctor about medications that can help with weight-loss. These medications are severely underutilized. There are different options, even if injectable medicines are too expensive for you. If your BMI is high, consider talking to a weight management clinic with experienced obesity physicians for help.
- Bariatric Surgery: If your BMI is higher than 35, bariatric surgery could be an option. Surgery can improve many chronic diseases, such as diabetes, and lower your cancer risk. The risks are similar to getting your gallbladder removed. Usually, the surgery takes around one hour, and you might spend one to two days in the hospital. Most people are back to work within 7 to 10 days.
Conclusion
Obesity is a chronic, relapsing disease that is difficult to treat. However, there are so many new treatment options now available to help. These new treatments are giving people with obesity a chance to feel better, have a better life, and lower their chances of getting cancer. We’re in a new time where treatments for obesity actually work and can make a big difference in health and happiness.
About the Authors:
Sarah Ro, MD, is a Lead Physician for the UNCPN Weight Management Program and is also an Adjunct Assistant Professor of Family Medicine at UNC School of Medicine. She is a Diplomat of the American Board of Obesity Medicine and helped create community-based weight management clinics in seven different communities in central North Carolina. This program has increased access to evidence-based obesity care for socially vulnerable populations most impacted by obesity.
Young Whang, MD, PhD, is the Associate Professor of Medicine, division of oncology, at the UNC School of Medicine, Chapel Hill, North Carolina. He is a medical oncologist with expertise in genitourinary cancers, such as prostate cancer. Dr. Whang’s research has been focused on the development of new cancer treatments and understanding how cancer develops.
by Nina Crowley, PhD, RD (with Inspiration from Shawn Cochran) Winter 2024 Dating, no matter your age,…
Read Articleby Leslie M. Golden, MD, MPH, ABOM Diplomate Winter 2024 The journey to overcoming obesity is a…
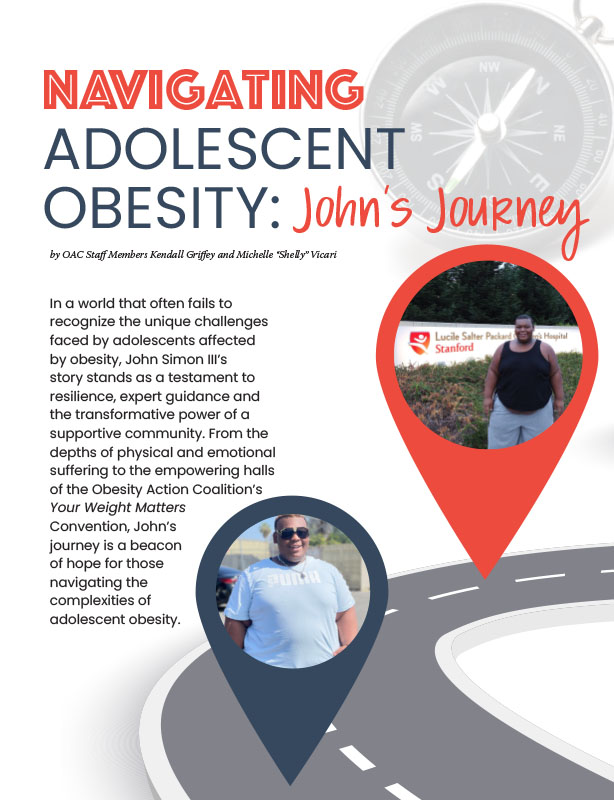
Read Articleby OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Article