Zepbound® — A New Treatment for Obesity

by Robert Kushner, MD
Spring 2024
Disclaimer: Before considering Zepbound®, consult with your healthcare provider.
In November 2023, the U. S. Food and Drug Administration (FDA) approved Zepbound® for chronic weight management. Zepbound® is the brand name for a once-weekly injection called Tirzepatide, available in 5 mg, 10 mg, and 15 mg doses. The medication is approved for adults with a body mass index (BMI) of 30 or higher or those with a BMI of 27 or higher and at least one weight-related medical condition.
What is Zepbound®?
Zepbound® is a prescription medication given by injection. It is intended for adults with obesity or excess weight who have weight-related medical problems to lose weight and keep it off. Medically, Zepbound® is a type of drug called a glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor dual-agonist that is engineered in a laboratory. This means Zepbound® mimics the two natural GIP and GLP-1 hormones that are released by the intestine into our bloodstream within minutes after we ingest food. These gut hormones do several important things in our bodies, including:
- Regulating blood sugar
- Slowing down how fast the stomach empties food
- Managing appetite
What Does the Research Show?
Research studies, called the SURMOUNT program, have looked into the effectiveness, safety, and tolerability of Zepbound®. The four studies involved around 5,000 people worldwide who were either affected by obesity or classified as overweight with co-existing weight-related medical problems.
Everyone in these studies was given advice on lifestyle changes and was randomly assigned (by the flip of a coin) to take either Zepbound® or a placebo, which is a substance with no real effect, for 72 to 88 weeks. The results of these studies were impressive. On average, people taking Zepbound® lost between 34 to 57 pounds. For someone weighing 230 pounds, this is significant weight-loss that can greatly improve their health. In the SURMOUNT-1 study, over one-third of people taking the 15 mg dose lost at least 25% of their weight.
The studies also showed significant improvements in:
- Waist circumference
- Blood pressure
- Blood fats
- Inflammation
- Physical ability
When Should Zepbound® Be Used?
Zepbound® should be used for the chronic management of obesity or overweight with an existing weight-related medical condition such as type 2 diabetes, hypertension, or sleep apnea. Like other medications approved for weight management, it should be taken alongside a healthy diet, regular physical activity, and behavioral counseling.
How is Zepbound® Administered?
Zepbound® is a self-injectable drug administered under the skin once weekly using a pre-filled pen injector. Patients start with a dose of 2.5 mg once a week for the first four weeks. After that, your dose will gradually increase every month until you find what works best for you, usually between 10 mg to 15 mg per week for most people. Increasing the dose slowly helps reduce the risk of side effects. Make sure to talk to your healthcare provider to figure out the best dosing schedule for you.
What Are the Side Effects of Zepbound®?
The most common side effects of Zepbound® include:
- Nausea
- Diarrhea
- Constipation
- Vomiting
Zepbound® may also cause hypoglycemia (low blood sugar) when used with other anti-diabetic drugs.
Are There Any Concerns About Zepbound®?
Zepbound® should not be used by patients who have had serious allergic reactions to tirzepatide or by those with a personal or family history of medullary thyroid carcinoma or a rare condition called Multiple Endocrine Neoplasia syndrome type 2 (MEN 2).
Zepbound® also contains warnings about:
Severe stomach issues
- Kidney damage
- Gallbladder problems
- Pancreatitis (inflammation of the pancreas)
- Changes in vision for people with type 2 diabetes
- Depression or thoughts of suicide
Conclusion
Zepbound® marks a new era in hormonal medications for chronic weight management that are more effective for weight-loss and for improving cardiovascular and metabolic health risks. Medications are an important tool in the medical management of obesity for many individuals. We expect that in the years to come, more highly effective medications will emerge, assisting those affected by obesity in their weight management journey.
About the Author:
Robert Kushner, MD, is a Professor of Medicine and Medical Education at Northwestern University Feinberg School of Medicine, and Director of the Center for Lifestyle Medicine at Northwestern Medicine in Chicago, IL. He is a founder of the American Board of Obesity Medicine (ABOM), past President of The Obesity Society (TOS), and past board member of the Obesity Action Coalition (OAC). Dr. Kushner has also served as the Chair and Co-Chair of the planning committee for OAC’s Your Weight Matters Annual Convention. Additionally, he serves on the Medical Advisory Board for Eli Lilly, for which he receives compensation.
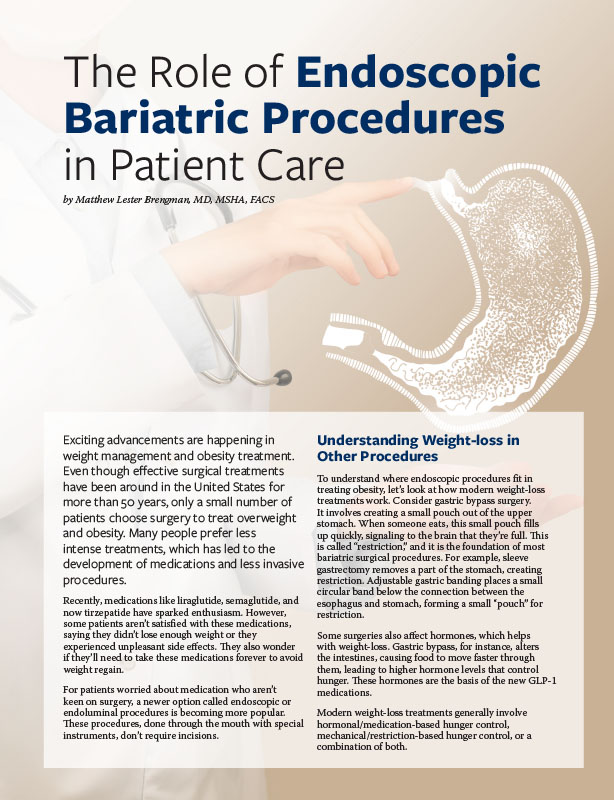
by Matthew Lester Brengman, MD, MSHA, FACS Spring 2024 Exciting advancements are happening in weight management and…
Read Articleby Craig Primack, MD, FACP, FAAP Fall 2013 Please Note: As of February 2020, the Food and…
Read Article