Your Health Matters: The Importance of COVID-19 Vaccines for Patients with Obesity

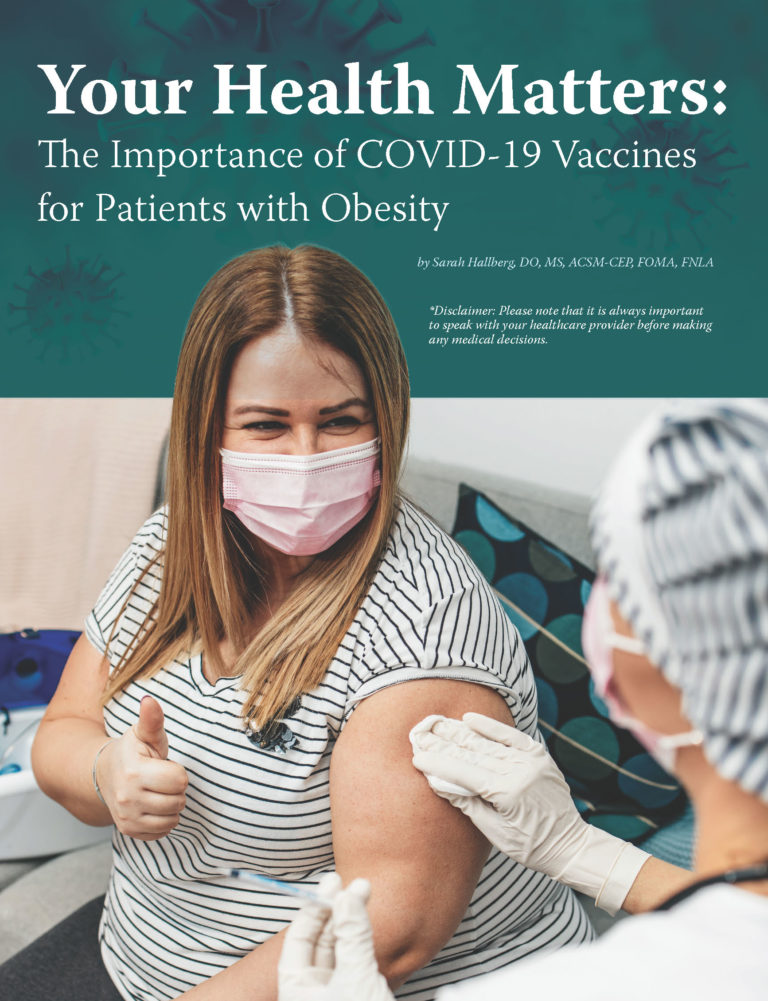
by Sarah Hallberg, DO, MS, ACSM-CEP, FOMA, FNLA
Summer 2021
*Disclaimer: Please note that it is always important to speak with your healthcare provider before making any medical decisions.
With the COVID-19 vaccine rollout accelerating across the United States, many people are beginning to see the light at the end of the pandemic tunnel. But while experts are constantly reminding everyone that COVID-19 is dangerous and that the vaccine can help eliminate some of those dangers, many people all over the world still remain skeptical about the vaccine.
Vaccine Prioritizing
Right now, it is too difficult to control the virus with the majority of the United States opening back up. This makes vaccination the only path to herd immunity and a resolution to this crisis. When the rollout of the vaccinations first began, experts made decisions about which groups of people would be given vaccine prioritization. They were broken down into vaccine “phases” and priority went towards elderly people and people with health conditions that could worsen the effects of COVID-19 if they were to contract it.
Decisions made during the vaccine rollout have prompted massive backlash — in particular, the fact that many states elected to prioritize vaccine access for people with obesity. Although the ultimate goal is — and should be — herd immunity, and although obesity has been shown to increase the risk of hospitalization and death in those who contract COVID-19, some people have suggested that struggling with obesity diminishes a person’s worthiness to receive the vaccine.
This is NOT true. Obesity is a chronic disease, not a choice or a failure of will, and prioritizing this population is the scientifically prudent thing to do. People affected by obesity deserve vaccine access because they are at an increased risk of becoming sick from COVID-19.
Weight Bias and Wellbeing
This backlash, unfortunately, is unlikely to come as a surprise to people living with obesity and clinicians who treat those affected by obesity. Weight bias is not a phenomenon isolated to vaccine rollout. Rather, it’s the single most common challenge patients struggling with weight issues experience. For those unfamiliar, weight bias refers to negative attitudes, judgements and stereotypes toward people managing excess weight or obesity — and it occurs nearly everywhere. From the classroom to the workplace — even in homes, social circles and yes, healthcare settings — weight bias is a widespread, negative force that creates shame and distress in those who experience it.
In the case of COVID-19, weight bias has prevented people in need from being vaccinated. People have shamed those affected by obesity and made them feel they are not worthy of being prioritized for the vaccine. People affected by obesity may feel too embarrassed to take advantage of their priority and opt out of their vaccination. In doing this, they are putting their lives and health at risk.
Weight bias should not prevent people from receiving the care that they deserve. It is crucial that people affected by obesity put their health first and don’t let the shaming of others dictate their health or the care that they receive. What is even more important is that weight bias is stopped and the disease of obesity is understood. To learn more about how you can help stop weight bias, visit StopWeightBias.com.
COVID-19 and Metabolic Disease
The past year has given everyone a greater understanding of the nature of viruses. We’ve become familiar with the outcomes associated with COVID-19 and the way it seems to roll off the shoulders of some while proving to be a catastrophic illness for others. In general, individuals with obesity or other metabolic diseases, such as diabetes, are at quite high risk for poor outcomes associated with coronavirus.
To summarize the findings, people with obesity have a 113% higher risk for hospitalization, a 74% higher risk for ICU admission and a 48% higher risk of death as a result of COVID-19, according to research from the University of North Carolina-Chapel Hill. Initially, it was thought that these results were due to correlations between obesity and other health risks, such as:
- Hypertension
- Heart disease
- Type 2 diabetes
- Chronic kidney disease
- Liver disease
As the pandemic has evolved, so has our understanding of the risks for people with obesity. Research has shown that people with obesity still deal with significantly greater risks related to COVID-19.
If those challenges were not enough, the pandemic has also created conditions of chronic stress, which can weaken immune systems and worsen obesity. In turn, this can aggravate other chronic conditions associated with obesity and complicate coronavirus recovery.
Vaccine Safety
The research is clear and so is the action we should take as a result. Those who are able to get the vaccine should strongly consider doing so. Providers must encourage their patients to get vaccinated as soon as possible. We must move the public conversation away from confusing a chronic disease with a choice. Every person deserves appropriate care and we must not allow weight bias and shaming to deter patients from gaining access to a vaccine that will protect them and strengthen our collective fight against the pandemic.
In the same way, it is important to reiterate that the various vaccines available in the United States have been proven safe and effective. With millions of doses already distributed, we should all feel more confident than ever that we are on the path to resolution with safe options. The fact that the Johnson & Johnson vaccine was halted and placed under investigation in the wake of potential blood clotting incidents has been presented with some alarm but should actually be a source of reassurance, proving that safety concerns and monitoring have been of the utmost importance throughout this process.
Vaccination is the best tool we have against the virus and it is critical for the health and wellbeing of anyone struggling with obesity or other metabolic diseases during this time.
Prioritizing Patient Health in the Pandemic and Beyond
This crisis has prompted each of us to reevaluate many elements of our lives: how we connect, how we work, how we live. Ideally, we’ll all come out of this more proactive about our health and wellbeing as well as the health and wellbeing of others. COVID-19 has proven to be a powerful reminder that we should all prioritize our health and reduce risks. Whether this means wearing a mask, getting vaccinated or prioritizing our physical and mental health in everyday living, we should all emerge from the situation as better advocates for ourselves. Likewise, providers should help every patient take action to live well and receive the care they need.
About the Author:
Sarah Hallberg, DO, MS, ACSM-CEP, FOMA, FNLA, is an internationally-recognized leader in the nutritional management of type 2 diabetes and other metabolic diseases. Dr. Hallberg founded IU Health Arnett’s Medically Supervised Weight Loss Program. She is the primary investigator for the largest and longest ever clinical trial examining a non-surgical intervention for the reversal of type 2 diabetes. Dr. Hallberg’s research has far-reaching implications for public health.
by Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Articleby Sarah Bramblette, MSHL Summer 2023 In the final months of 2022, I experienced both the worst…
Read Article