Why You Shouldn’t Delay Your Medical Appointments

by Angela Fitch, MD
Spring 2017
You only have one life to live – don’t delay!
pro · cras · ti · nate – “to put off intentionally the doing of something that should be done; the avoidance of a task that should be accomplished.”
Approximately 80 percent of us do it on a regular basis. We do it with putting off cleaning the stove, repairing our car, seeing a doctor or dentist, preparing a job presentation or academic assignment, or discussing a stressful issue with a friend. Procrastination can lead to feelings of guilt, inadequacy, depression and anxiety. To a certain degree, it is normal to procrastinate. It can be a useful coping tool to identify what is important because most people tend to procrastinate less on truly valued tasks.
Why Do We Procrastinate?
Procrastination is an inherently human behavior. Other mammals don’t do it, so why do we? The theory is that procrastination arose as a by-product of impulsivity. The more impulsive someone is, the more likely they are to put off those tasks that don’t provide immediate gratification and do other rewarding things instead. No one likes to do things they perceive as not giving them a reward. In our current society, there are so many things that give us instant gratification – so why would we do something where the reward is not instantaneous, and the task may be painful or challenging?
Your Health Matters!
It’s important that you don’t delay creating a beneficial relationship with your healthcare team. Support from a healthcare team can bring you so much reward in the long term! It’s typically not an instant reward, and it can sometimes be painful. Sometimes you have to talk about difficult issues, and sometimes you have to do difficult things and face your fears – fear of death, fear of disease, or the fear of something that’s not right. Denial is a powerful motivator of procrastination.
If we wait too long while living in denial, we miss an opportunity to live better, healthier and fuller lives! Our current healthcare system is more of a disease care system. We wait until the last minute to seek medical attention for something because:
- We are either too busy or don’t have the transportation to attend appointments.
- We’re not allowed to take off work.
- We can’t find a provider to take our insurance.
Many of these situations are real problems that we must abolish if we want to switch from a disease care system to a healthcare system!
Everyone Deserves to be Well
We all deserve to have a medical home where we can turn to for the best health and wellness care. This should be a place where you can form a relationship with a medical home, a team of providers (nurses, lab techs, medical assistants, patient service representatives, health coaches, dietitians, nurse practitioners, physician assistants, and physicians), and a place that knows what health risks and challenges you face in your wellness journey. If we form these relationships when we are well, then we can work on preventing diseases and identifying others early in the process. This allows us to take action so that we can change the outcome or improve our overall quality of life.
“Good things happen to those who wait” is NOT the mantra when it comes to addressing medical issues. If we wait too long, any disease or issue we might have may be too far along and not as effectively treatable. Or, if it is treatable, it may be more painful or even decrease your quality of life. These days, we are living longer and longer – and we not only want to live long, but we want to have a good quality to that length of life.
Making Healthcare Work for YOU
Patients tell me all the time that they assumed I would “yell” at them for their weight, poor eating habits, sedentary behavior, blood sugar levels, blood pressure or poor sleep. Why do we assume people will “scold us?” Why is life always about the negative and punishing behavior? We inherently do not like to see or hear about something which we are doing wrong. This is called the pleasure principle – or our instinctive drive to seek pleasure and avoid pain – but we have to balance that principle with unpleasant (or perceived as unpleasant, such as going to the doctor) tasks.
Healthcare systems are working to make the experience of accessing healthcare more pleasing. This includes a more pleasant waiting room, shorter wait times, virtual care, walk-in care and online scheduling – just to name a few. Stepping on the scale or getting an injection are situations that are harder to make pleasant, but we can offer tools and resources instead of criticism. This is what is most beneficial.
Weight bias in the world is very real, and it can lead to a delay in care. There are lots of discussions about this important issue, and even healthcare centers are sometimes guilty (though often not intentionally). Talk to your healthcare team about your concerns and be open and honest about your feelings and needs. They might not realize if there is a problem. For instance:
- If it is hard to get out of the chairs, tell someone.
- If the phone system was challenging to navigate, tell someone.
- If the gowns are too small, tell someone.
This will take a team effort and a patient-centered medical home to make progress, but together we can!
Are You Procrastinating?
Check Out these Tips if You Find Yourself Procrastinating Medical Care:
- Practice Mindfulness – Be aware of habits and thoughts that lead to your decision to procrastinate your care.
- Seek Out Help – Seek out help for self-defeating problems such as fear, anxiety, difficulty concentrating, poor time management, indecisiveness and perfectionism.
- Evaluate Yourself – Take a look at your own goals, strengths, weaknesses and priorities.
- Set realistic goals – Develop a personal and positive link between the tasks and your concrete, meaningful goals. Think of all the good reasons that you should be part of a medical “home.”
- Restructure Your Priorities – Reorganize your daily activities so that you can put yourself first when needed. Yes, your child may have soccer practice – but you cannot take them to practice if you are not around to do so.
- Take Your Time – Tackle issues in small blocks of time instead of trying to solve whole problems at once. When you make your appointment, be sure to talk with the scheduling staff to ensure that you will have enough time with the provider to meet your needs. Realize that you may need to address issues in a prioritized manner because you can’t always cover it all in one sitting.
- Examine Your Options – Shop around and get advice from friends to find a care team that you feel comfortable working with.
- Stay Up-to-date – Sign-up for the healthcare team’s electronic reminders or patient portal (take MyChart with the Epic Systems electronic medical record, for example). Get a text reminder for your appointments.
- Be Prepared – Go into your provider’s office with a specific agenda and tell them what you are hoping to accomplish at the visit. What do you want to get from that day’s appointment?
Conclusion
If you delay care for your car, you can either pay the price for repair or buy a new one. If you delay care for your body, you only have one of those options. You can’t buy a new body, so take care of the one you have!
Put your feet, fingers and forks to use for good and consider following my “5 P’s for a Healthy Life” – planned portions, mostly plants and protein, doing something powerful with your muscles each day and respecting your pillow with a good night’s sleep!
About the Author:
Angela Fitch, MD, is an Associate Professor of Internal Medicine at the University of Cincinnati College of Medicine. Board-certified in pediatrics, internal medicine and obesity medicine, she is the VP of UC Health Primary Care and serves as the Director of Medical Weight Management at the UC Health Weight-loss Center. She is a Board Trustee for the Obesity Medicine Association. Dr. Fitch developed an interest in obesity medicine after years of treating patients with obesity and related complications in primary care, and finding this to be an area not adequately addressed in general practice. Her commitment to focus on practicing in the field of obesity medicine was solidified when she completed her training and board certification from the American Board of Obesity Medicine.
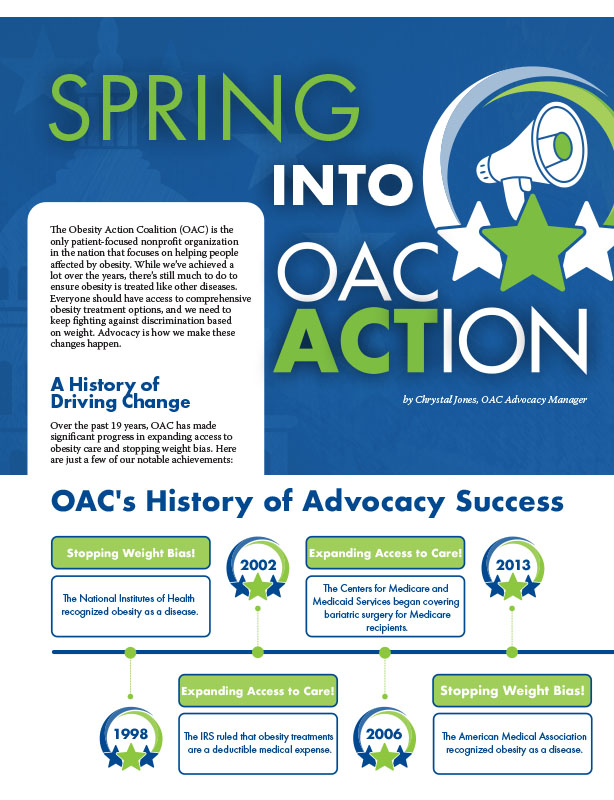
by Chrystal Jones, OAC Advocacy Manager Spring 2024 The Obesity Action Coalition (OAC) is the only patient-focused…
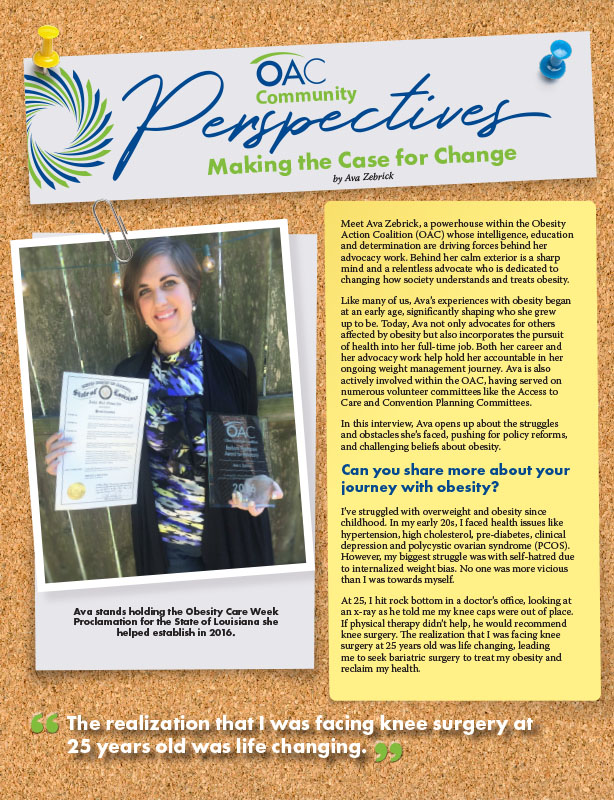
Read Articleby Ava Zebrick Spring 2024 Meet Ava Zebrick, a powerhouse within the Obesity Action Coalition (OAC) whose…
Read ArticleThe OAC is honored to welcome three new members to the OAC National Board of Directors. Jason Krynicki,…
Read Article