Type 2 Diabetes & Obesity: Can We Treat Diabetes through Obesity Treatments?

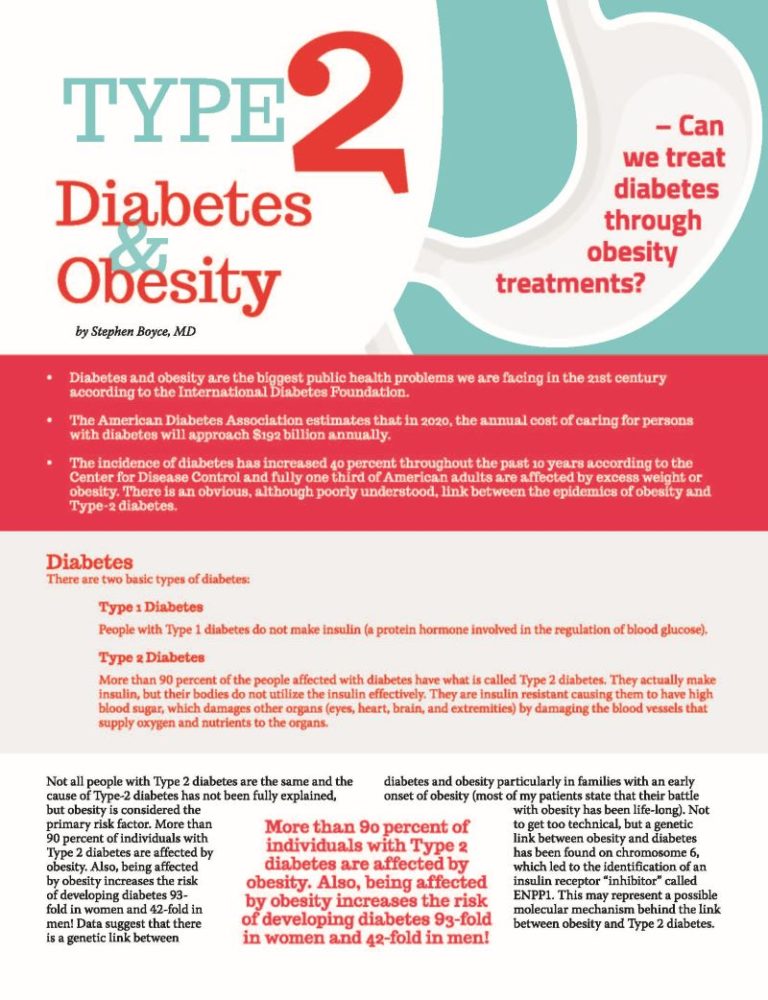
by Stephen Boyce, MD
Spring 2015
- Diabetes and obesity are the biggest public health problems we are facing in the 21st century according to the International Diabetes Foundation.
- The American Diabetes Association estimates that in 2020, the annual cost of caring for persons with diabetes will approach $192 billion annually.
- The incidence of diabetes has increased 40 percent throughout the past 10 years according to the Center for Disease Control and fully one third of American adults are affected by excess weight or obesity. There is an obvious, although poorly understood, link between the epidemics of obesity and Type-2 diabetes.
Diabetes
There are two basic types of diabetes:
Type 1 Diabetes
People with Type 1 diabetes do not make insulin (a protein hormone involved in the regulation of blood glucose).
Type 2 Diabetes
More than 90 percent of the people affected with diabetes have what is called Type 2 diabetes. They actually make insulin, but their bodies do not utilize the insulin effectively. They are insulin resistant causing them to have high blood sugar, which damages other organs (eyes, heart, brain, and extremities) by damaging the blood vessels that supply oxygen and nutrients to the organs.
Not all people with Type 2 diabetes are the same and the cause of Type-2 diabetes has not been fully explained, but obesity is considered the primary risk factor. More than 90 percent of individuals with Type 2 diabetes are affected by obesity. Also, being affected by obesity increases the risk of developing diabetes 93-fold in women and 42-fold in men! Data suggest that there is a genetic link between diabetes and obesity particularly in families with an early onset of obesity (most of my patients state that their battle with obesity has been life-long). Not to get too technical, but a genetic link between obesity and diabetes has been found on chromosome 6, which led to the identification of an insulin receptor “inhibitor” called ENPP1. This may represent a possible molecular mechanism behind the link between obesity and Type 2 diabetes.
Type-2 diabetes is a progressive disease (like severe obesity) and the natural history is one of progressive loss of insulin secretion throughout time due to the loss of cells in the pancreas (beta cells) that make and secrete insulin. This leads to the need for more intense therapy with multiple medications. The human toll of diabetes and severe obesity are truly frightening. It is estimated that the combination of the two diseases results in a loss of healthy life of 12-24 years for women and 16-32 years for men.
Treatment
A number of treatment regimens exist for diabetes and as with all chronic diseases, the most appropriate treatment depends on the severity of the disease. There are many effective medications that are commonly used; unfortunately, they may cause obesity to worsen. A number of these medications used to treat diabetes actually cause people to gain weight, worsening their diabetes, sleep apnea, hypertension and cholesterol. Medicines that are known to be associated with weight gain include:
- Insulin
- Glyburide
- Glimepiride
- Glipizide
- Pioglitazone
- Rosiglitazione
These drugs are commonly used to treat Type 2 diabetes because they are so effective. It can feel like a no-win situation.
There is Good News, Though!
First, modest weight-loss improves the sensitivity to insulin, thus improving diabetes. Of course, we know that obesity is also a chronic progressive disease and that maintaining significant weight-loss throughout time is rare, especially for the person who suffers from severe obesity.
Second, metabolic and bariatric surgery (sleeve gastrectomy, Roux-en-Y gastric bypass [RNYGB], and biliopancreatic diversion with duodenal switch [BPD/DS]) has been shown to be better than maximal medical therapy for treating diabetes in people who suffer from obesity of all classes (mild, moderate and severe obesity).
The mechanism for Type 2 diabetes resolution after metabolic surgery is interesting. After metabolic surgery, there is an increase in the production of compounds (called incretins) that increase the number of cells in the pancreas that secrete insulin. Incretins have also been shown to restore the body’s response or sensitivity to insulin. These powerful compounds result in diabetes improvement and even complete resolution even before the benefits of weight-loss have been realized. Studies have shown that metabolic surgery is more effective than maximal medical therapy even in people who suffer from mild to moderate obesity (BMI 30-35). This is truly a radical finding!
With respect to diabetes resolution, not all treatment options are equal. Diabetes resolution rates for:
- Medical therapy
- Sleeve Gastrectomy
- RNYGB
- BPD/DS
- 0%
- 70%
- 80%
- 95%
Unfortunately, the results are not always permanent. People with longstanding diabetes (on insulin more than 10 years), and those with poorly controlled diabetes before bariatric surgery seem to be at risk for recurrence of their diabetes after RNYGB. BPD/DS is generally accepted to have the most durable effect on resolution of diabetes in people affected by the disease.
Perhaps as important, metabolic surgery has been shown to prevent the development of diabetes in people with impaired glucose tolerance. Impaired glucose tolerance is a precursor to Type 2 diabetes.
As a bariatric surgeon, I love helping patients resolve their life-threatening obesity-related diseases like Type 2 diabetes, but, whether it is through metabolic bariatric surgery or through lifestyle and behavioral modification, it doesn’t matter. Weight-loss resolves Type 2 diabetes for a happier, longer, healthier life.
About the Author:
Stephen Boyce, MD, obtained his Bachelor of Science and Masters of Science from Texas A&M University, College Station, before beginning medical school in Dallas, Texas at the University of Texas Southwestern Medical School where he received his medical degree. Surgical Residency was performed at Parkland Memorial Hospital in Dallas where he completed his general surgery training. With more than 24 years of experience performing bariatric surgeries, Dr. Boyce has completed more than 4,000 bariatric surgical procedures, has special training in advanced laparoscopic surgery and has also completed a Masters Certification in Bariatric Surgery. He started his own practice, the New Life Center for Bariatric Surgery, in Knoxville, Tenn. in 2002, which shortly after became one of the Nation’s first Centers of Excellence (7th in the Nation) in 2005. His special interest in bariatric nutrition led him to develop Bari Life Bariatric Supplements, specializing in custom multivitamin formulas for the bariatric surgery patient. Additionally, he is an active educator for Ethicon-Endo Surgery and a two-time recipient of the OAC’s “Dr. Blackstone Outstanding Membership Recruitment by a Physician” award.
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read Articleby Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Article