The Post-surgery Diet for Bariatric Patients: What to Expect

By Denise Addorisio, RD, CDN
Spring 2009
Have you decided to have bariatric surgery, or are you post-op and on your way to losing weight? That’s great, but first you need to understand the basic principles of the post-op diet, for either laparoscopic adjustable gastric banding (LAGB) or Roux-en-Y gastric bypass, so you can properly use the tool the surgeon has created for you.
First and foremost, remember that your overall dietary goal is to optimize the nutritional value of the small portions of foods you eat so you get the nutrients your body needs to be healthy. Portion sizes for meals should be no more than six to eight ounces total, and this should make you feel full or at least “satisfied.”
If you had LAGB and you can eat more than that amount comfortably, you may be due for a fill. But, whether you had LAGB or gastric bypass, you must develop an awareness of your body’s signals of satisfaction, and be in tune with your body’s early feelings of fullness.
Nutrients – It’s all about Protein
Protein is the most important nutrient in the bariatric diet. Foods high in protein should be eaten first, in case you feel full and cannot finish your meal. While the best sources of proteins are eggs, poultry, meats, fish, cheese and milk, other protein sources to consider include beans, lentils and soy products such as soy burgers.
Red meats such as beef, pork, lamb or veal can be particularly difficult for a bariatric patient to digest. Be sure to choose tender cuts, but watch out for the potential for higher fat content (that means higher calories). Some bariatric programs encourage regular use of protein supplements, but your best choice is always traditional foods unless you have a particular situation that requires you to add protein supplements to your diet. Suggested long-term post-op protein intake may range from 55-80 grams per day.
Because starches such as bread products, rice and pasta can be trigger foods for many formerly patients with obesity, many bariatric programs limit their intake. Although carbohydrates are your body’s primary fuel source, carbohydrates are also found in fruits and vegetables. Unfortunately, many patients have had limited intakes of fruits and vegetables in their pre-op diet and never consciously thought about their importance to a balanced diet, which is even more important now. Each meal should contain at least one fruit or vegetable, or perhaps one serving of each.
Starches such as bread products, rice and pasta are also carbohydrates. Because these types of carbohydrates can be trigger foods for many patients with obesity, some bariatric programs limit their intake. Tolerance of these foods may also be an issue, though tolerance may improve with time. Choose whole grain breads and choose brown rice and whole grain/high protein pasta if you do decide to include them in your diet.
Helpful Tips and Guidelines
Check your portion sizes.
Use measuring tools and a food scale to check your portion sizes. Serving meals on smaller plates, such as salad or luncheon plates, will help make these small portions look more appealing.
Eat three meals each day.
Eating three meals each day helps to prevent snacking or
“grazing,” which can add many calories between meals. Most long-term post-op bariatric patients find they need to limit their total caloric intake to less than 1,000 calories per day to maintain their weight-loss.
Eat slowly.
Foods should be eaten slowly. Since most bariatric patients were fast eaters in their previous life, this can be a difficult behavior to change. Use tools such as small baby spoons and forks to help slow you down. An egg timer is a handy way of making sure that you wait two minutes between bites, which helps you stretch the meal period to the suggested 20 to 30 minutes.
Chew your food carefully.
Chewing your food carefully, perhaps up to 15-20 chews per bite, until the foods feels pureed before swallowing, will help slow you down. It is also important to chew foods well to ensure that nothing gets stuck passing through the narrowed outlet from the pouch. Failure to eat small portions, eat slowly and chew carefully can lead to vomiting, which is never considered normal.
Dumping with Gastric Bypass vs. LAGB
Some types of bariatric surgeries, such as gastric bypass, create a situation where dumping occurs if the post-op patient eats sweets such as cake, cookies or ice cream. The aspect of the gastric bypass surgery that creates malabsorption through bypassing part of the intestine is the reason for dumping. These symptoms may include abdominal pain, nausea, diarrhea, dizziness and hot flashes or cold sweats.
For most patients, knowing they will become sick after eating sweets will be a strong deterrent, preventing them from wanting to eat those foods. However, if you eat “just a bite” of sweets over time, you can build up a tolerance for them. This means that you will eventually be able to eat more sweets without experiencing dumping, and then only willpower will help you avoid these high fat, high sugar, high calorie foods. Of course, that can ultimately lead to regaining of weight or perhaps not even reaching your expected weight-loss.
While dumping can be a strong deterrent to sweets for gastric bypass patients, LAGB patients will find they can tolerate sweets since their gastrointestinal tract remains intact. For the LAGB patient with a sweet tooth, calories will add up quickly if they are not careful to limit the portions and frequency of sweets. Remember, sweets usually provide little nutritional value in terms of protein, vitamins and minerals, so reading labels for calorie content and controlling portions is key.
Fluids
Fluids are an important part of any diet, but particularly for the bariatric patient. All liquids should be consumed between meals, never with a meal. Again, this can be a hard habit to break, but it is very important to your success.
Drinking with meals can lead to “pushing” the solid food through your pouch more quickly, which leads to faster emptying of your pouch. When your pouch is empty, you feel hungry. The sooner your pouch is empty, the hungrier you will feel and you will be tempted to eat between meals.
Choose fluids that are non-carbonated. Yes, that means no soda – diet or regular. Besides making you feel uncomfortable, the gas produced by the carbonated beverage can stretch the pouch or its outlet. Stretching means that you will soon be able to fit larger portions of foods in your pouch before you feel full. Remember, more food equals more calories.
Your best choices for fluids are water (try squeezing lemon in there); artificially sweetened, non carbonated beverages such as Crystal Lite® and Diet Snapple®; flavored waters; decaf coffee or tea; herbal teas; broth; and diluted 100 percent fruit juices. Read labels carefully to be sure your healthy “vitamin water” is not loaded with calories. And, do not forget that alcoholic beverages are full of calories with no nutritional value.
Vitamins and Minerals
All bariatric patients need to take vitamin and mineral supplements as recommended. While the amounts and types of supplements may vary by their bariatric program and specific type of surgery, professionals agree that these supplements are necessary to prevent vitamin and/or mineral deficiencies.
Both LAGB and gastric bypass patients need to take multiple vitamin and mineral supplements daily for the rest of their lives. Bypass patients require additional supplements of iron, calcium and Vitamin B-12 due to malabsorption created by the bypass portion of their surgery.
But no matter which surgery you had, regular, periodic lab tests should be monitored annually or semi-annually to ensure that you are meeting your nutritional needs. Of course, proper dietary choices are important in this respect as well.
Your goal should be to get as much of the needed vitamins and minerals from foods first by making wise food choices that maximize nutritional value while keeping calories low. That means your diet should include lots of whole grains, low-fat dairy products, fruits and vegetables, as well as adequate protein.
Conclusion
Having a good understanding of proper nutrition is critical for the success of bariatric surgery. Consult your dietitian regularly to learn all you need to properly use the tool that the surgeon has given to you.
About the Author:
Denise Addorisio, RD, CDN, is a registered dietitian specializing in bariatric surgery and weight management. She provides pre and post-op nutritional consultations for New York Bariatrics and is also an adjunct professor of nutrition at Westchester Community College in New York.
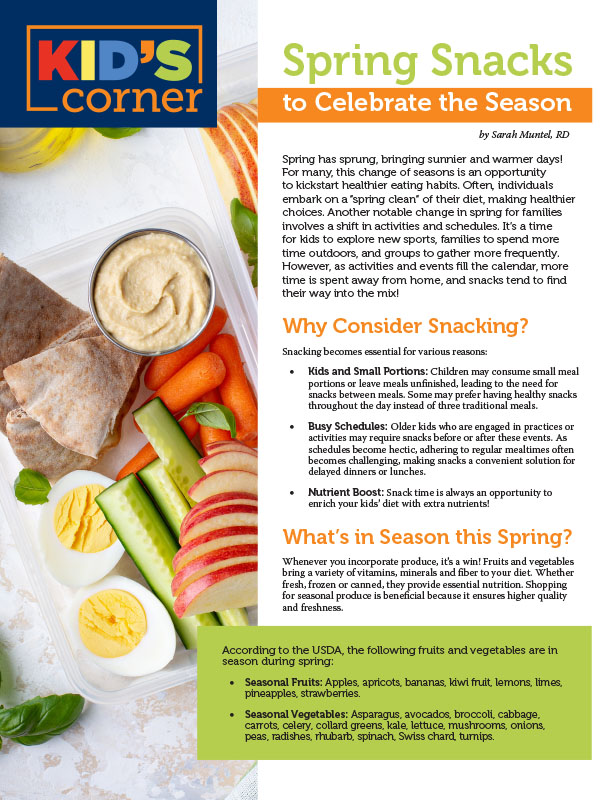
by Sarah Muntel, RD Spring 2024 Spring has sprung, bringing sunnier and warmer days! For many, this…
Read Articleby OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Article