The Importance of the Essential Health Benefits (EHB) Package

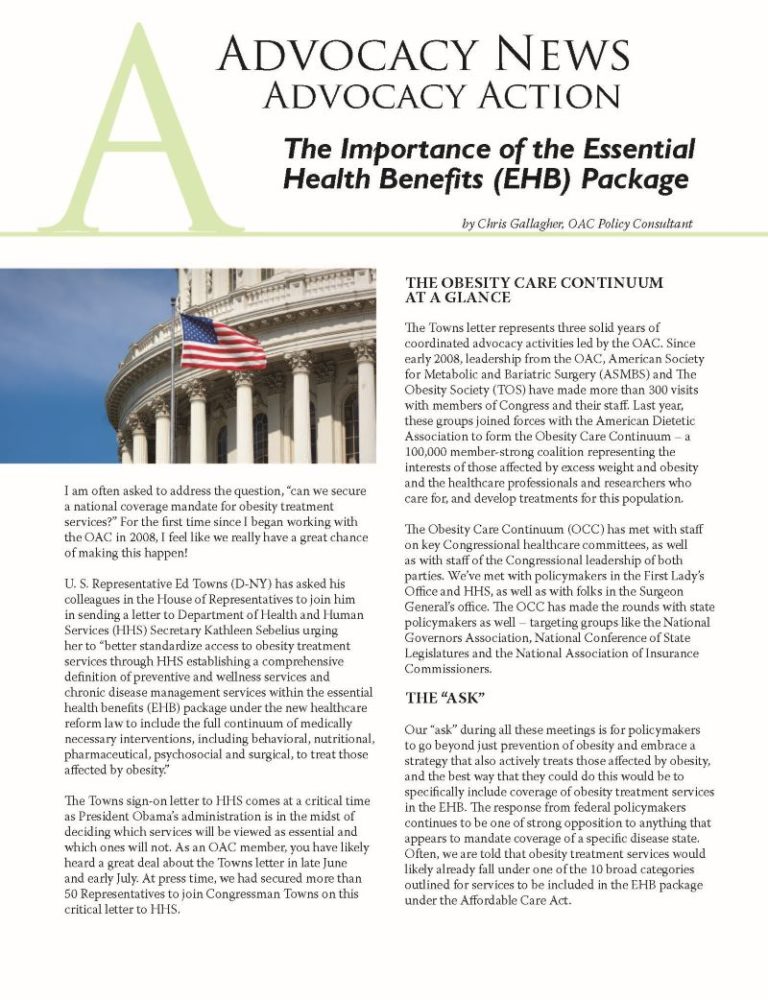
by Chris Gallagher, OAC Policy Consultant
Summer 2011
I am often asked to address the question, “can we secure a national coverage mandate for obesity treatment services?” For the first time since I began working with the OAC in 2008, I feel like we really have a great chance of making this happen!
U. S. Representative Ed Towns (D-NY) has asked his colleagues in the House of Representatives to join him in sending a letter to Department of Health and Human Services (HHS) Secretary Kathleen Sebelius urging her to “better standardize access to obesity treatment services through HHS establishing a comprehensive definition of preventive and wellness services and chronic disease management services within the essential health benefits (EHB) package under the new healthcare reform law to include the full continuum of medically necessary interventions, including behavioral, nutritional, pharmaceutical, psychosocial and surgical, to treat those affected by obesity.”
The Towns sign-on letter to HHS comes at a critical time as President Obama’s administration is in the midst of deciding which services will be viewed as essential and which ones will not. As an OAC member, you have likely heard a great deal about the Towns letter in late June and early July. At press time, we had secured more than 50 Representatives to join Congressman Towns on this critical letter to HHS.
The Obesity Care Continuum at a Glance
The Towns letter represents three solid years of coordinated advocacy activities led by the OAC. Since early 2008, leadership from the OAC, American Society for Metabolic and Bariatric Surgery (ASMBS) and The Obesity Society (TOS) have made more than 300 visits with members of Congress and their staff. Last year, these groups joined forces with the American Dietetic Association to form the Obesity Care Continuum – a 100,000 member-strong coalition representing the interests of those affected by excess weight and obesity and the healthcare professionals and researchers who care for, and develop treatments for this population.
The Obesity Care Continuum (OCC) has met with staff on key Congressional healthcare committees, as well as with staff of the Congressional leadership of both parties. We’ve met with policymakers in the First Lady’s Office and HHS, as well as with folks in the Surgeon General’s office. The OCC has made the rounds with state policymakers as well – targeting groups like the National Governors Association, National Conference of State Legislatures and the National Association of Insurance Commissioners.
The “Ask”
Our “ask” during all these meetings is for policymakers to go beyond just prevention of obesity and embrace a strategy that also actively treats those affected by obesity, and the best way that they could do this would be to specifically include coverage of obesity treatment services in the EHB. The response from federal policymakers continues to be one of strong opposition to anything that appears to mandate coverage of a specific disease state. Often, we are told that obesity treatment services would likely already fall under one of the 10 broad categories outlined for services to be included in the EHB package under the Affordable Care Act.
Policymakers would say, “Surely umbrella categories like ambulatory patient services and hospitalization would cover medical weight management and bariatric surgery. Surely, the prescription drug category would include coverage for FDA-approved obesity drugs. And if not those areas, surely treating obesity would fall under the ‘preventive and wellness services and chronic disease management’ section of the benefit package.”
Our response to these assurances has been, “not so fast.” For starters, the vast majority of individual and small health plans specifically exclude anything having to do with obesity or weight-loss programs. Second, there is still quite a great deal of debate, even within the healthcare community, as to whether or not obesity is really a disease. And lastly, many policymakers believe that prevention alone will solve the obesity epidemic.
While the OAC believes that prevention is critically important, there also needs to be a good balance between preventing more people from becoming affected by obesity and helping those who currently struggle with their weight. Focusing solely on prevention, without a corresponding push for the treatment side of the equation, writes off nearly two-thirds of our population already affected by excess weight or obesity.
Following the Footsteps of Mental Health and Substance Abuse Services
What is really needed is an approach similar to the one that was taken with mental health and substance abuse services, which by the way, ARE specifically mentioned as a covered category of services under the healthcare reform law. Why are these services carved out for special consideration? Shouldn’t they also fall under hospitalization, ambulatory care, prescription drugs, or the wellness umbrellas? They’re clearly enumerated because of the pervasive discrimination and stigma that was, and still continues, to be associated with mental illness and addiction.
How did the mental health community pull it off? I can assure you it didn’t happen overnight. It took years, decades if you will, of tireless lobbying by the mental health community to educate not only policymakers, but more importantly, their peers in the medical community – some of which still scoff at those who struggle with mental illness or addiction as “defective” or “weak.”
Our approach before Congress, HHS and the White House is that obesity is deserving of the same consideration as mental illness due to the same societal hurdles that face those seeking treatment for the disease of obesity.
Just as the mental health community was successful in their battle to protect access to, and coverage of, specific treatment services from health plan bias and discrimination, so will we in our campaign! However, if we are going to win the day, the swell of support for this cause must grow strong and must grow fast! When it comes to the EHB, either you’re in or you’re out. Let’s all work together so we end up on the inside looking out for a change!
Essential Health Benefits Package
Mandated Categories of Covered Services:
- ambulatory patient services
- emergency service
- hospitalization
- maternity and newborn care
- mental health and substance abuse disorder services, including behavioral health treatment
- prescription drugs
- rehabilitative and habilitative services and devices
- laboratory services
- preventive and wellness services and chronic disease management pediatric services, including oral and vision care
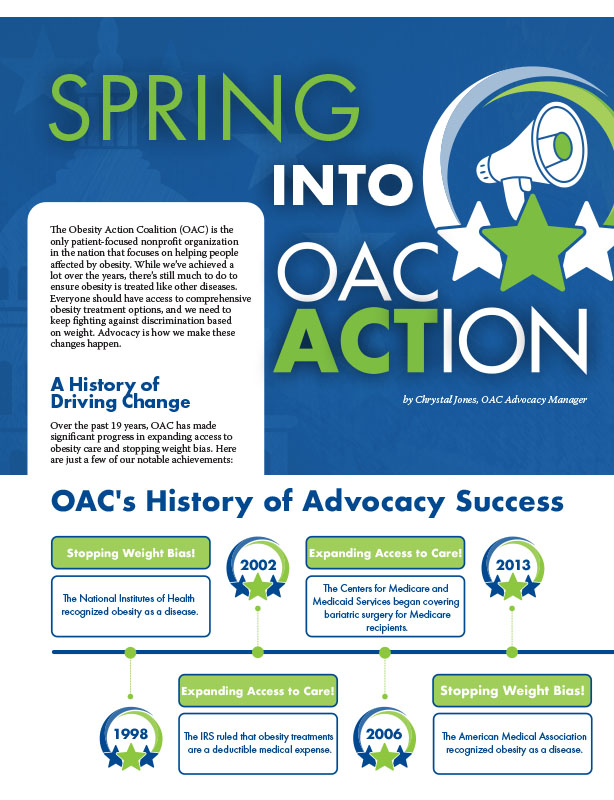
by Chrystal Jones, OAC Advocacy Manager Spring 2024 The Obesity Action Coalition (OAC) is the only patient-focused…
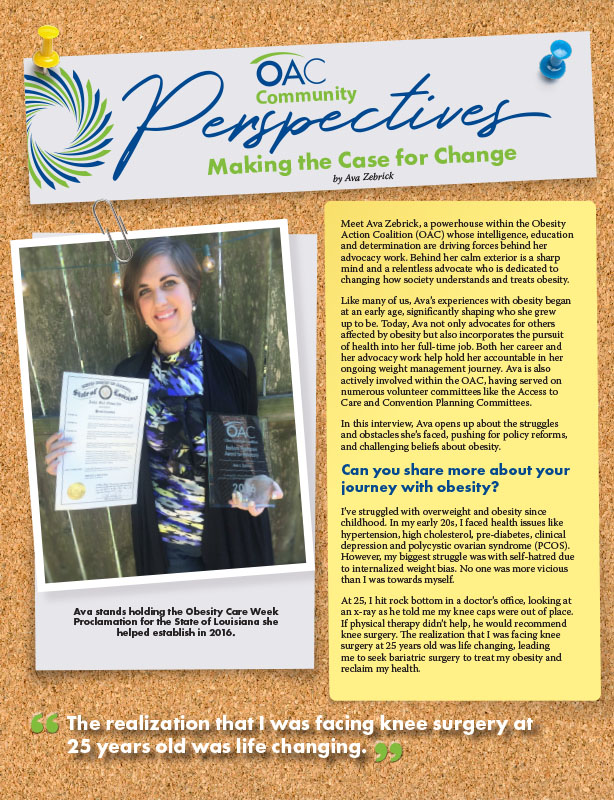
Read Articleby Ava Zebrick Spring 2024 Meet Ava Zebrick, a powerhouse within the Obesity Action Coalition (OAC) whose…
Read ArticleThe OAC is honored to welcome three new members to the OAC National Board of Directors. Jason Krynicki,…
Read Article