Obesity and Osteoarthritis Fact Sheet
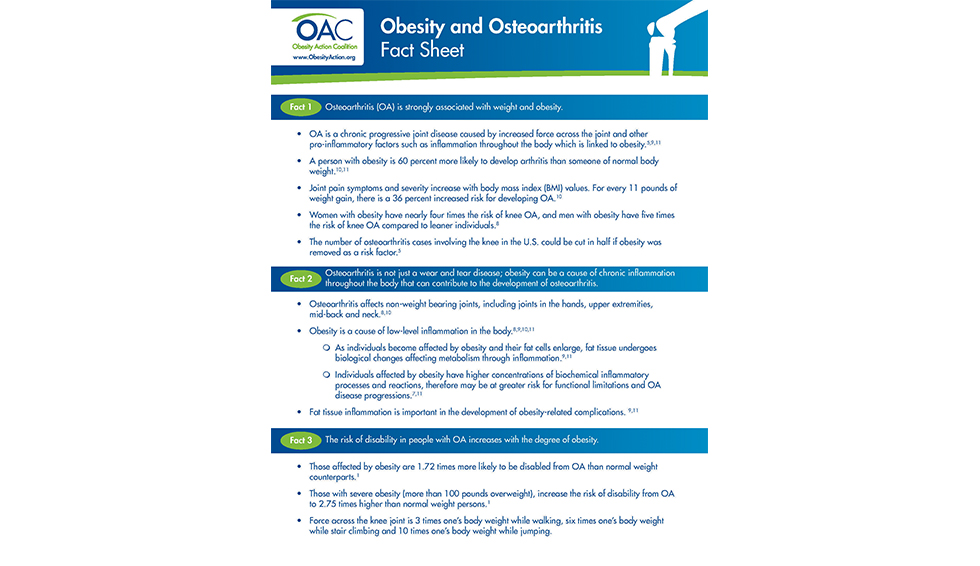
Osteoarthritis (OA) is strongly associated with weight and obesity.
- OA is a chronic progressive joint disease caused by increased force across the joint and other pro-inflammatory factors such as inflammation throughout the body which is linked to obesity.
- A person with obesity is 60 percent more likely to develop arthritis than someone of normal body weight.
- Joint pain symptoms and severity increase with body mass index (BMI) values. For every 11 pounds of weight gain, there is a 36 percent increased risk for developing OA.
- Women with obesity have nearly four times the risk of knee OA, and men with obesity have five times the risk of knee OA compared to leaner individuals.
- The number of osteoarthritis cases involving the knee in the U.S. could be cut in half if obesity was removed as a risk factor.
Osteoarthritis is not just a wear and tear disease; obesity can be a cause of chronic inflammation throughout the body that can contribute to the development of osteoarthritis.
- Osteoarthritis affects non-weight bearing joints, including joints in the hands, upper extremities, mid-back and neck.
- Obesity is a cause of low-level inflammation in the body.
- As individuals become affected by obesity and their fat cells enlarge, fat tissue undergoes biological changes affecting metabolism through inflammation.
- Individuals affected by obesity have higher concentrations of biochemical inflammatory processes and reactions, therefore may be at greater risk for functional limitations and OA disease progressions.
- Fat tissue inflammation is important in the development of obesity-related complications.
The risk of disability in people with OA increases with the degree of obesity.
- Those affected by obesity are 1.72 times more likely to be disabled from OA than normal weight counterparts.
- Those with severe obesity (more than 100 pounds overweight), increase the risk of disability from OA to 2.75 times higher than normal weight persons.
- Force across the knee joint is 3 times one’s body weight while walking, six times one’s body weight while stair climbing and 10 times one’s body weight while jumping.
Weight-loss can reduce joint pain and symptoms of osteoarthritis; obesity is the most modifiable risk factor for OA.
- For women with obesity, for every 11 pounds of weight lost, the risk of knee osteoarthritis drops more than 50 percent.
- Weight-loss can significantly improve the symptoms of patients with osteoarthritis by restoring function and quality of life and preventing more than 100,000 total knee replacements each year.
- Intensive weight-loss will reduce inflammation and joint loads sufficiently to alter disease progression.
- Both exercise training and weight-loss decrease overall inflammation.
- Weight-loss helps prevent the onset of OA symptoms and disability.
- Obesity (BMI ≥ 30.0 kg/m2) is associated with increased risk of functional impairment and is considered the most modifiable risk factor for knee OA.
Please note: While BMI is commonly used to screen for obesity, it has its limitations and does not replace clinical judgment. BMI is not a direct measure of body fat and does not consider muscle mass, bone mass or fat distribution. Social determinants, race, ethnicity and age may modify the risk associated with a given BMI. An elevated BMI increases your risk for overweight and obesity, but only a healthcare provider can make the final determination.
by Sarah Muntel, RD Summer 2024 Here comes summer with sunshine, relaxation and lots of fun! As…
Read Articleby Nina Crowley, PhD, RD Summer 2024 Before we talk about body composition, it’s important to know…
Read Articleby Greer Raggio, PhD, MPH Summer 2024 When we think about grief, we often imagine someone coping…
Read Article







