Medicare and Bariatric Surgery: Are We Better off Today?


Fall 2007
In February 2006, to much public acclaim, Medicare announced an expansion of its coverage of bariatric surgery. As we look at this ruling nearly more than a year and a half later, a harsh reality becomes evident. Bariatric surgery, in many parts of the country, is no more available today to Medicare beneficiaries than it was prior to the ruling.
Understanding Medicare Coverage
Under Medicare, the Centers for Medicare and Medicaid Services (CMS), the agency that oversees Medicare, hires regional contractors (usually insurance companies) to determine benefit coverage and pay claims for Medicare beneficiaries. The vast majority of decisions on coverage are made at the local level by the regional contractors and not by Medicare itself.
Under this system, prior to February 2006, Medicare coverage for bariatric surgery varied widely. In some parts of the country, coverage was widely available, while in others it was non-existent.
The National Coverage Decision
With this disparity in mind, leaders of the American Society for Metabolic and Bariatric Surgery (ASMBS) along with many others, asked CMS to make a National Coverage Determination (NCD) regarding the surgical treatment of morbid obesity. An NCD requires that all Medicare contractors follow the same ruling. The intent of the NCD was to level the field by applying the same guidelines regarding the availability to and requirements for bariatric surgery.
After a very lengthy and intensive process, a positive NCD was released by Medicare validating bariatric surgery as a safe and effective treatment for morbid obesity and including a number of guidelines, some specific and some vague, regarding both the availability and requirements for bariatric surgery.
The Problem: Regional Contractors Continue to Limit Access
The NCD should have been the solution and granted widespread access to bariatric surgery to appropriately selected candidates, but it hasn’t.
The problem is that the vague guidelines have allowed the regional contractors to interpret and administer the guidelines. As a result, some regional contractors are now developing their own criteria for certain requirements to access bariatric surgery (also called local coverage determination, or LCD). And these requirements, in the opinion of the OAC, are vastly limiting access to care. (Please see the chart below for examples of how some regional contractors interpret the NCD.)
Adding to the challenge is also what seems to be a lack of agreement between CMS and the Medicare contractors on who determines and interprets coverage policies. Examples of such vagueness and how Medicare contractors are interpreting the NCD:
EXAMPLE 1
Medicare NCD States: Previously unsuccessful with medical treatment for obesity
Medicare Contractor Interpretation through LCD Coverage Policy: Documented evidence of repeated failure of multiple attempts (usually 3) of at least 6 months each to lose weight on a supervised non-surgical management weight-loss program. (Contractor with this requirement: Cigna Government Services)
EXAMPLE 2
Medicare NCD States: Have at least one co-morbidity related to obesity
Medicare Contractor Interpretation through LCD Coverage Policy: Specifically defining co-morbidities. For example, hypertension (defined as blood pressure of 140 mmHg systolic and/or 90 mmHg diastolic) despite medical treatment with maximal doses of three antihypertensive medications. (Contractor with this requirement: Trailblazer Health)
Working to Improve Access
So how do we improve coverage? The OAC, in partnership with the ASMBS and others, is actively fighting this battle on many fronts. First, we continue to work with Medicare and CMS and advise them of major challenges patients experience accessing care.
We have begun working with the Medicare contractors advising them if we believe their policies are unfair or lack scientific basis. To date, we have had some limited success with the Medicare contractors but also have been told by some that they are not interested in revising their policies. As a result, we are now also considering further action on both the legal and legislative front to force local intermediaries to follow the spirit of the NCD.
Improving Medicare Access is Important
Medicare issuing an NCD was just the first step. We must actively continue to ensure that Medicare beneficiaries have access to bariatric surgery. Why is it so important? Remember that most commercial insurers follow Medicare’s lead when it comes to coverage and policies. As such, fixing Medicare’s coverage not only helps Medicare beneficiaries but also all of those seeking to access treatment for their morbid obesity.
OAC’s Call to Action
If you have been personally affected by a Medicare contractor’s LCD or have been unable to access bariatric surgery under Medicare, please share your story with us by calling (800) 717-3117 or e-mailing us at info@obesityaction.org. We need to hear from you so we can share your story with Medicare as well as others supporting our efforts to improve care.
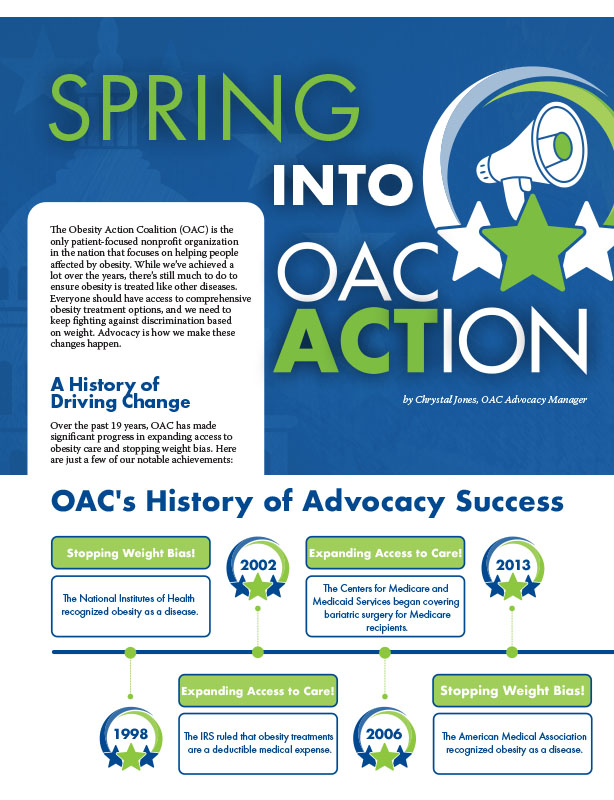
by Chrystal Jones, OAC Advocacy Manager Spring 2024 The Obesity Action Coalition (OAC) is the only patient-focused…
Read Articleby Ava Zebrick Spring 2024 Meet Ava Zebrick, a powerhouse within the Obesity Action Coalition (OAC) whose…
Read ArticleThe OAC is honored to welcome three new members to the OAC National Board of Directors. Jason Krynicki,…
Read Article