Making the Most of Healthcare: The Patient-Provider Partnership


by Patty Nece, JD; and Scott Kahan, MD, MPH
Winter 2019
A Cycle of Doubt and Shame: Patty’s Story
Years ago, in one of many efforts to lose weight, a dietitian prescribed for me an 1800 calorie “exchange” program with specific servings of specific foods each day. She told me what I was permitted to eat, what foods were “good” and “bad” and to eat three strict meals daily with nothing in between.
I carefully followed her regimen and lost 20 pounds. Success, right? However, I constantly craved “forbidden” foods and woke each night with severe hunger pangs. I couldn’t think of anything but food. I sacrificed the foods I enjoyed and avoided social situations for fear of temptation. I felt terrible and knew I couldn’t keep it up.
My dietitian was sympathetic, but wouldn’t budge from her rules or her theory that my body would adjust. She offered no options or guidance. I stayed the course for a bit longer and “white-knuckled” through cravings and deprivation. Eventually, I gave in. I felt ashamed and alone. I soon regained all the weight – plus quite a bit more.
I’ve repeated this so many times – whether working with a dietitian, doctor, or following low-carb or low-fat plans. We’ve all been there: A well-meaning healthcare professional lays down the law about what we can and can’t do, what we should and shouldn’t eat, what’s “right” and what’s “wrong.” You leave with a black and white set of instructions and swear that you’ll follow it. But if you’re anything like me, you end up in the same place you started – feeling entirely hopeless.
An Obesity Clinician’s Perspective: Dr. Scott Kahan
When I met Patty, I was instantly intrigued. She was wickedly smart, hardworking, very successful and just plain lovely. Common stereotypes of people with obesity suggest they are lazy or have no willpower – just the opposite of what I saw in Patty. These and other antiquated beliefs about obesity imply that healthcare providers should be stern and uncompromising – barking at patients to work harder and motivating change via harsh rules and requirements.
This is wrong. “Tough love” doesn’t motivate. Most of my patients beat themselves up enough. We must all understand that obesity is complex and managing weight is extremely challenging for most people because of the environmental, social and biological factors that influence weight gain. While hard work is important for any goal, this isn’t simply an issue of willpower – nor is there a magic diet plan or simple answer that will easily cure obesity.
Patty had been beaten down by her weight, her diets, lifelong weight stigma, shaming and more. She didn’t need to be pushed into yet another unsustainable diet plan.
When it comes to weight management, it’s not the clinician’s job to tell patients what to do. Instead, we should support them to build the skills and confidence to take charge of their health:
- Approach each person with genuine curiosity to appreciate who they are and what’s meaningful to them.
- Listen and learn about their goals, strengths and challenges.
- Empower them to find their motivations and help them build a plan to fit their lives and preferences.
- Offer unwavering support as they work toward their goals, and problem-solve with them through any challenges.
This isn’t to say that discussing diets, medical treatments or other recommendations is inappropriate. But, we should offer our expertise in a collaborative manner so that our patients have the information and confidence they need to advocate for themselves.
A New Experience in Healthcare: When Patty Met Scott
The first thing that struck me when I met Dr. Scott Kahan was that he never judged or blamed me for my weight. That was a new experience for me – and incredibly refreshing.
Still, I was concerned that he didn’t immediately make me follow a diet plan. Scott had a different approach. (By the way, he doesn’t like to be called “Dr. Kahan,” and I now appreciate why: I always feel like we’re partners – working together to help me improve my health. He’s not an authoritarian telling me what to do.)
We talked for more than an hour – about my job, family, past experiences and why I wanted to lose weight. He listened to my concerns and goals. We went over my medical and weight history. He taught me about the science of obesity and how our bodies can fight against weight-loss. He told me there were dozens of science-based options I could try. I even learned about the potential benefits and drawbacks of structured diets, as well as why they work for some people but not others.
Scott never pushed me. Though I’d been prepared to start another strict diet, I soon realized this was actually the last thing I wanted. Instead, I felt more confident to take some other steps.
Together, we agreed to start with a few small changes:
- Adding small, satiating snacks into my day.
- Treating a severe vitamin D deficiency.
- Paying attention to my thoughts and emotions in relation to food choices.
I also left with my next appointment already scheduled – and for the first time, I actually looked forward to it! Even after a single meeting, I felt that Scott would be unconditionally supportive of me, regardless of how I was doing or how many pounds I lost. Nothing was more valuable to me.
A Note about Shared Decision Making
Shared decision making (SDM) is a partnership between a patient and a healthcare provider so patients can make treatment decisions that fit their goals, interests and preferences. Physicians and other healthcare providers should be open-minded and patient-centered, aiming to:
- Help patients understand the nature of their health conditions and the pros and cons of different treatments.
- Ensure patients have the right information to make informed decisions.
SDM keeps the patient at the center of care. Patients share their values, preferences, needs and concerns. Treatment decisions are made together. Studies show that SDM leads to improved adherence to treatments and greater patient satisfaction1.
SDM is important because no one can tell you what you’re all about, what you want, what drives you or what your goals are. SDM may feel awkward at first – but does it ever feel good to be told what to do without your input?
Patty: Carving My New Path
At first, I wondered if Scott felt that I wasn’t strong enough to follow a strict diet plan. What I didn’t realize then is what Scott really gave me: a way to take control for myself. He was there to support this process – not take it over. It’s like he and his team were pieces of the puzzle, but I was the puzzle-maker. I just needed confidence to take charge.
By actively participating in decisions about my weight and health, I became empowered to make changes that felt right for me. I felt more energy than ever before to go down a new path. I ultimately lost more than 100 pounds and have kept if off for years – something I never thought was possible.
I wish I could go back in time to when I met with that dietitian. I’d insist on being heard and having my needs addressed. If she refused, I’d look elsewhere to find a better fit – someone who would partner with me. I luckily found that partnership with Scott.
To learn more about Patty and Scott’s work together, read their HealthCentral.com article at:
https://immersive.healthcentral.com/obesity/d/LBLN/btg-obesity-patty-nece/flat/.
Looking for a healthcare provider to help you manage your weight? Visit OAC’s Obesity Care Provider Locator at: ObesityCareProviders.com.
Characteristics of Clinicians Who Practice Shared Decision Making:
- Approaches the topics of weight and health in a non-judgmental way.
- Listens to your needs, concerns, goals and preferences.
- Conveys details about all relevant treatment options, such as benefits and risks, rather than just giving a prescription.
- Encourages you to ask questions so that you fully understand your options.
About the Authors:
Patty Nece, JD, is an active member of the Obesity Action Coalition (OAC) Community. She serves on the OAC Board of Directors and Chairs OAC’s Weight Bias Task Force. A passionate advocate, she shares her life-long experience with obesity to advocate against weight bias and to support science-based obesity treatments.
Scott Kahan, MD, MPH, is a physician trained in clinical medicine and public health. Dr. Kahan is the Director of the National Center for Weight and Wellness in Washington, DC and Chair of the Clinical Committee for The Obesity Society. He serves on the Board of Directors for the OAC, the American Board of Obesity Medicine, The Obesity Society and the Obesity Treatment Foundation.
References:
- Katz SJ, Hawley S. The value of sharing treatment decision making with patients. JAMA 2013; Sept E1-E2.
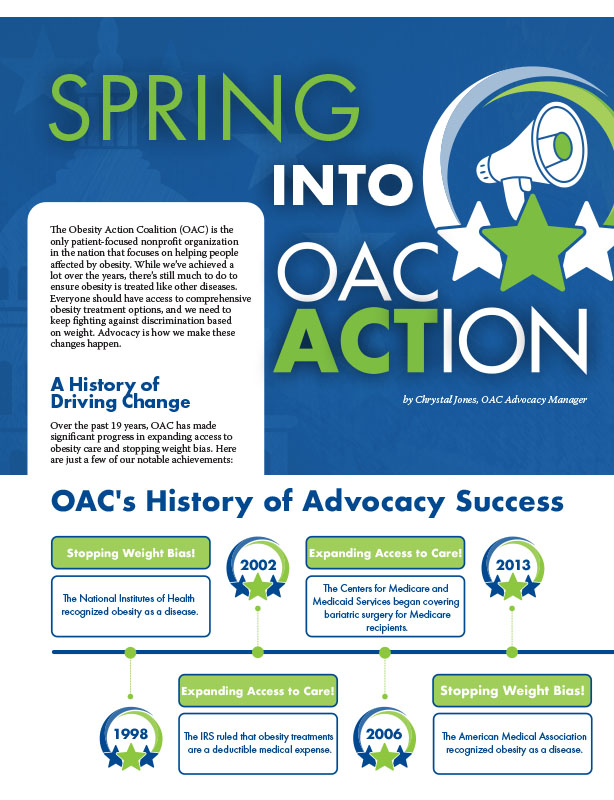
by Chrystal Jones, OAC Advocacy Manager Spring 2024 The Obesity Action Coalition (OAC) is the only patient-focused…
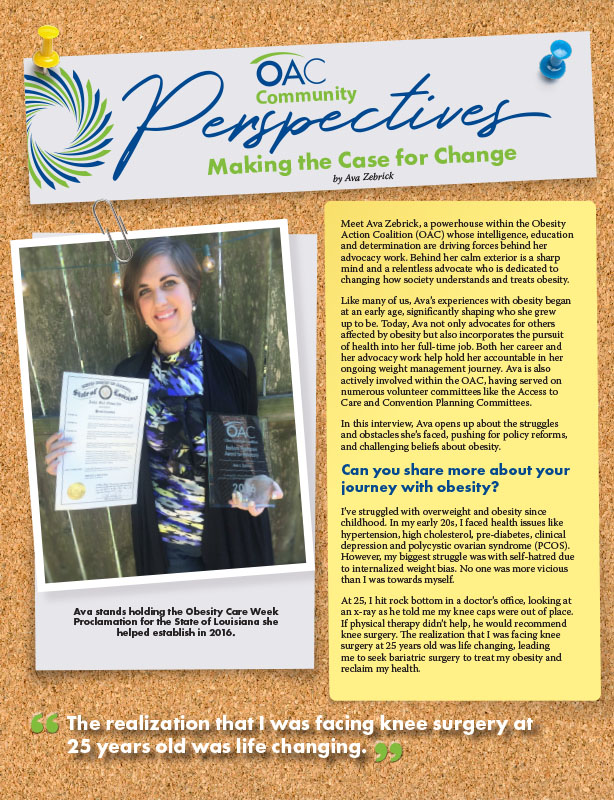
Read Articleby Ava Zebrick Spring 2024 Meet Ava Zebrick, a powerhouse within the Obesity Action Coalition (OAC) whose…
Read ArticleThe OAC is honored to welcome three new members to the OAC National Board of Directors. Jason Krynicki,…
Read Article