Don’t Judge a Book by its Cover: My Experience with Obesity, Autism and Rare Disease

by Maxie McGlohon, MSN, RN, FNP, LNC, Rare Disease Advocate
Fall 2020
I’ll never forget one evening when I attended a dinner at a medical meeting with a large group of couples. Like myself, all the women were wives of doctors. I was sitting at the other end of the table when I overheard a conversation between two of them. “I just have zero tolerance for obese people!” one of them exclaimed. She was implying that all people with obesity lack willpower and simply choose to be heavy.
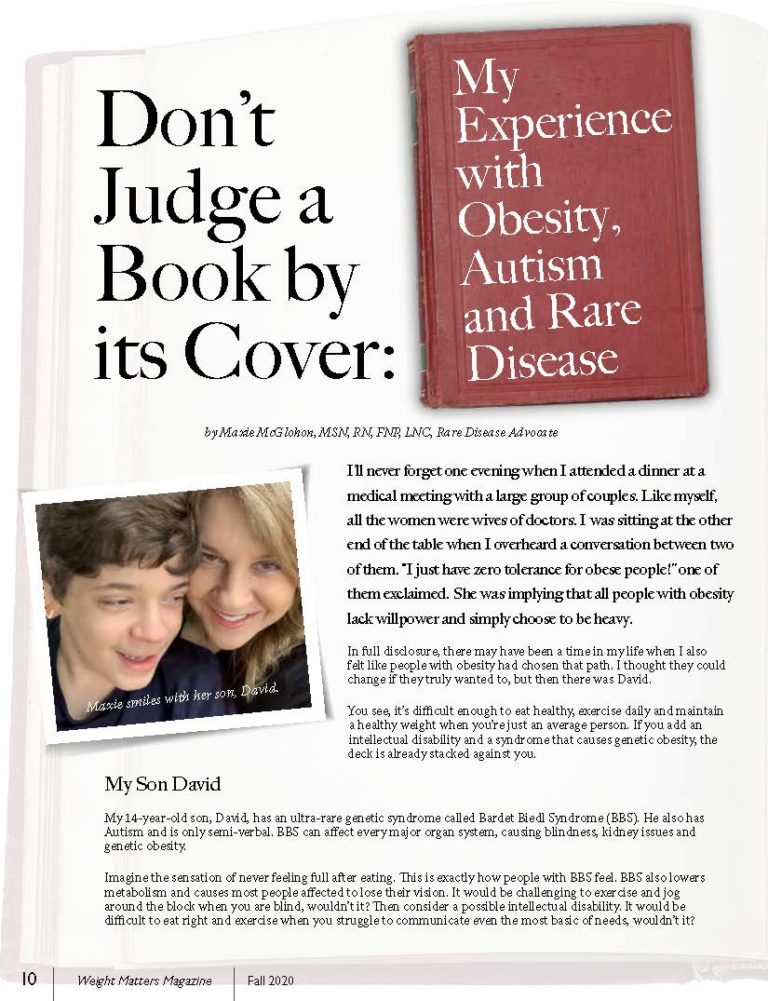
In full disclosure, there may have been a time in my life when I also felt like people with obesity had chosen that path. I thought they could change if they truly wanted to, but then there was David.
You see, it’s difficult enough to eat healthy, exercise daily and maintain a healthy weight when you’re just an average person. If you add an intellectual disability and a syndrome that causes genetic obesity, the deck is already stacked against you.
My Son David
My 14-year-old son, David, has an ultra-rare genetic syndrome called Bardet Biedl Syndrome (BBS). He also has Autism and is only semi-verbal. BBS can affect every major organ system, causing blindness, kidney issues and genetic obesity.
Imagine the sensation of never feeling full after eating. This is exactly how people with BBS feel. BBS also lowers metabolism and causes most people affected to lose their vision. It would be challenging to exercise and jog around the block when you are blind, wouldn’t it? Then consider a possible intellectual disability. It would be difficult to eat right and exercise when you struggle to communicate even the most basic of needs, wouldn’t it?
An Honest Reflection
I mentioned earlier that there was once a time when I truly didn’t “get it.” I am a nurse practitioner, and I’ve worked in family practice for years. I have diagnosed and treated many patients with hypertension, diabetes, high cholesterol, kidney issues, heart disease and other health conditions. Many of these patients had obesity.
At every appointment, we would discuss healthy diet and exercise. Most of them had follow-up visits every three months. I remember one time, after seeing a patient for years, he came in with a blood sugar level that was higher than ever. I felt like I was failing. I wondered, “Why couldn’t he get his blood sugar and weight down?”
This had been a particularly difficult day, and I treat every patient like they are my family. This is how I would want to be treated. Where was I failing him because he wasn’t losing weight? I got frustrated, so I started telling him that this was going to affect his heart and kidneys and that he was going to die if he didn’t get control of his health.
Later, I felt terrible for talking so directly with him. But again, my patients are my family and I didn’t want my family member to die. It never really crossed my mind that he might have a genetic reason for his obesity. Not once. I thought he should just eat healthy and exercise more.
Learning from Experience
Unfortunately, most people seem to have this mindset. Over the years, my position has certainly changed! Since my son was diagnosed, I’ve met many children and adults affected by genetic obesity. I’ve heard their stories about being bullied and discriminated against, their struggles with depression, and about questioning their self-worth. It’s heartbreaking.
If more healthcare providers as well as the general public could just fully understand genetic obesity, perhaps there would be more:
- Compassion
- Support systems
- Research
- Acceptance
Caring for My Son
So, how do you care for a child with autism, an intellectual disability and a rare syndrome to address their physical, mental and emotional health? How do you help them exercise and attempt to maintain a healthy weight? Trust me, this isn’t easy. It’s a struggle that weighs on my heart daily.
My son’s BBS specialist informed us that even though his weight is normal and stable at this time, his genetic weight issues may still catch up with him. All of the exercise in the world may one day not be able to keep the weight gain from attacking my son. How do you say “no” when your child is lying on the floor, kicking and screaming, begging for food, even though they have already eaten three full meals and two snacks? They simply don’t feel full and are still hungry. My son constantly asks for food and is always hungry. My husband and I truly try our best to help him be healthy.
Most of the time, when David is crying for food, we try to redirect him with a range of outdoor activities:
- Walking
- Riding bikes
- Jumping on the trampoline
- Playing on the swing or play set
My son absolutely loves to swim, so we purchased a small above-ground pool from Walmart. This was the best investment we ever made! It’s such great exercise for him and he can work on his physical training and occupational therapy goals in the water.
You may be saying, “I don’t have the finances for such things,” but exercise is something you can do anywhere and anytime. Here are some examples:
- Walk in a park
- Walk up and down stairs in your house or apartment
- Rake leaves in the yard
- Work in the garden
- Do anything that gets you moving and your heart pumping!
As far as diet goes, we try very hard not to have any “junk food” in the house. My whole family struggles with temptation and trying to maintain a healthy weight. We try to only keep healthy options in the kitchen such as fresh fruit and veggies, lean meats, nuts and healthy carbs. We also try to eat organic when we can. When David is screaming for a snack, we try to offer an apple, banana or orange instead of cookies and chips. He also loves veggies, so we often spiralize raw veggies like carrots and zucchini. He loves the shape and actually asks for these!
Now again, in full disclosure, life sometimes gets in the way. We don’t always adhere to our diet as we should and we sometimes splurge too much. Still, that doesn’t mean we don’t want our son to lead as normal of a life as possible.
On a daily basis, David eats as recommended by his health specialist:
- Gluten-free
- Dairy-free
- Low-sodium
- Low-carb
- Low-calorie
However, if David is at school or somewhere special, and they are having a cake for someone’s birthday party, we let him have the cake with gluten. We occasionally get his all-time favorite food: pizza. We simply try to increase his activity later that day. He also needs to drink at least two liters of water daily, as urged by his kidney doctor, which has the added benefit of helping him curb his appetite.
With everything, our goal is moderation. While we are hopeful and optimistic about David’s future, we still try to be realistic – especially about the likelihood of his vision loss. We try to engage him in activities that he can do even if he goes blind. The best example is swimming, and thank goodness that’s his favorite thing to do.
We also take him to participate in other activities:
- Adaptive surfing
- Surfer’s healing
- Adaptive waterskiing
- Adaptive snow skiing
- Horseback riding
Taking care of David’s emotional and mental health can be challenging, but we try to take things one day at a time. David participates in speech and occupational therapies. Since my husband and I are both musically inclined, we do our very own music therapy as often as we can with our busy lives. My son really seems to find his voice in music. He struggles to do everything in life, so we try to help him find his voice wherever we can. We mainly just give him all of the love we have for him: lots of high-fives, snuggles, hugs and kisses.
The World I’m Fighting for
I hope my story can help even one person understand more about genetic obesity. The next time you see someone with obesity or excess weight, don’t judge. Don’t judge when you see that mom in the grocery store with her heavier child, putting cake and sodas in her cart. They may be trying hard to live a healthy lifestyle, but may just be celebrating a child’s birthday. Don’t make assumptions that they are lazy and eat too much.
Try to remember these things:
- Some people can’t help that they struggle with weight
- Some people may have issues in their life contributing to weight gain
- We’re all different
- Compassion goes a long way
Try not to judge a book by its cover, because if you do, you may be missing out on some very special and beautiful people.
About the Author:
Maxie McGlohon, MSN, RN, FNP, LNC, Rare Disease Advocate, wears many hats. She is a family nurse practitioner, legal nurse consultant, rare disease advocate for the Bardet Biedl Syndrome (BBS) Foundation and all rare diseases, and a mother as well as case manager to her son, David, who has BBS and Autism. Mrs. McGlohon emphasizes that she will never stop believing in her son and all that he can do in this world.
To connect with Maxie, you can click here for her Facebook and here for her Instagram. She is a published author and updates her blog often. To follow her journey, please click here.
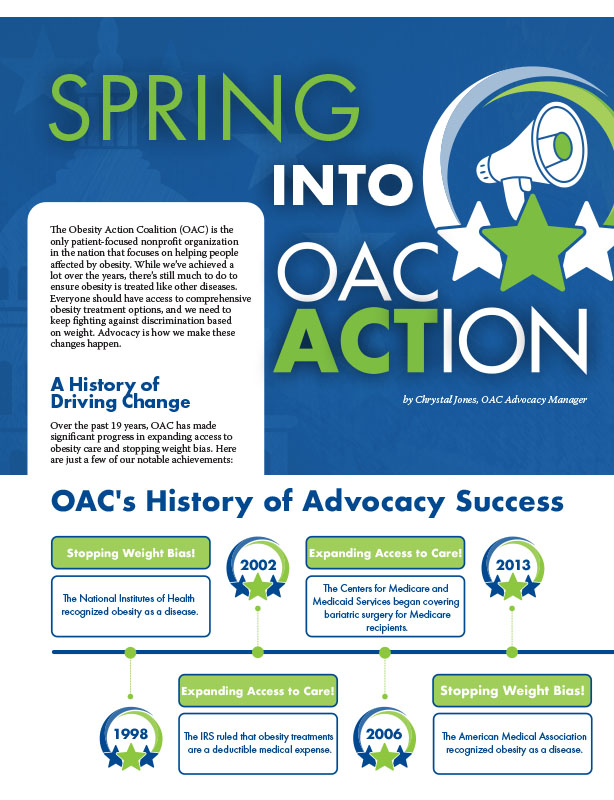
by Chrystal Jones, OAC Advocacy Manager Spring 2024 The Obesity Action Coalition (OAC) is the only patient-focused…
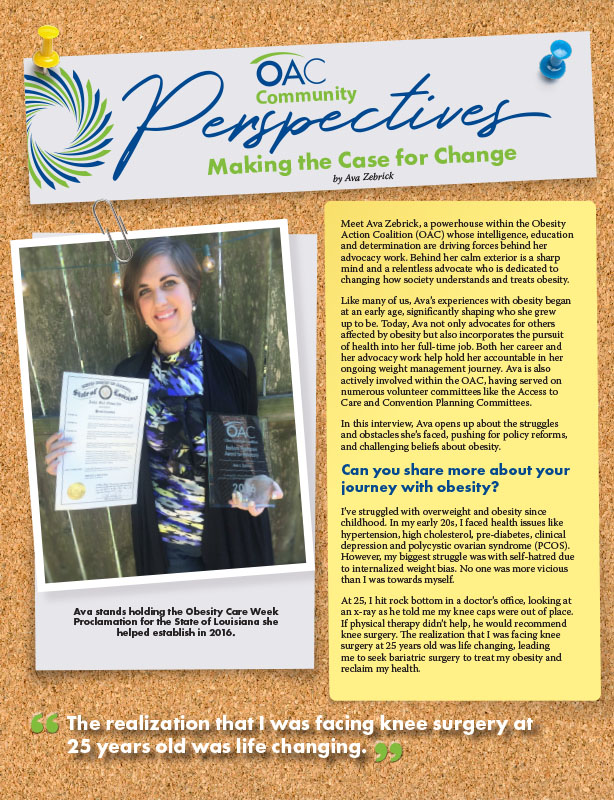
Read Articleby Ava Zebrick Spring 2024 Meet Ava Zebrick, a powerhouse within the Obesity Action Coalition (OAC) whose…
Read ArticleThe OAC is honored to welcome three new members to the OAC National Board of Directors. Jason Krynicki,…
Read Article