Dear Doctor: My child is gaining weight, and I don’t know what to do.

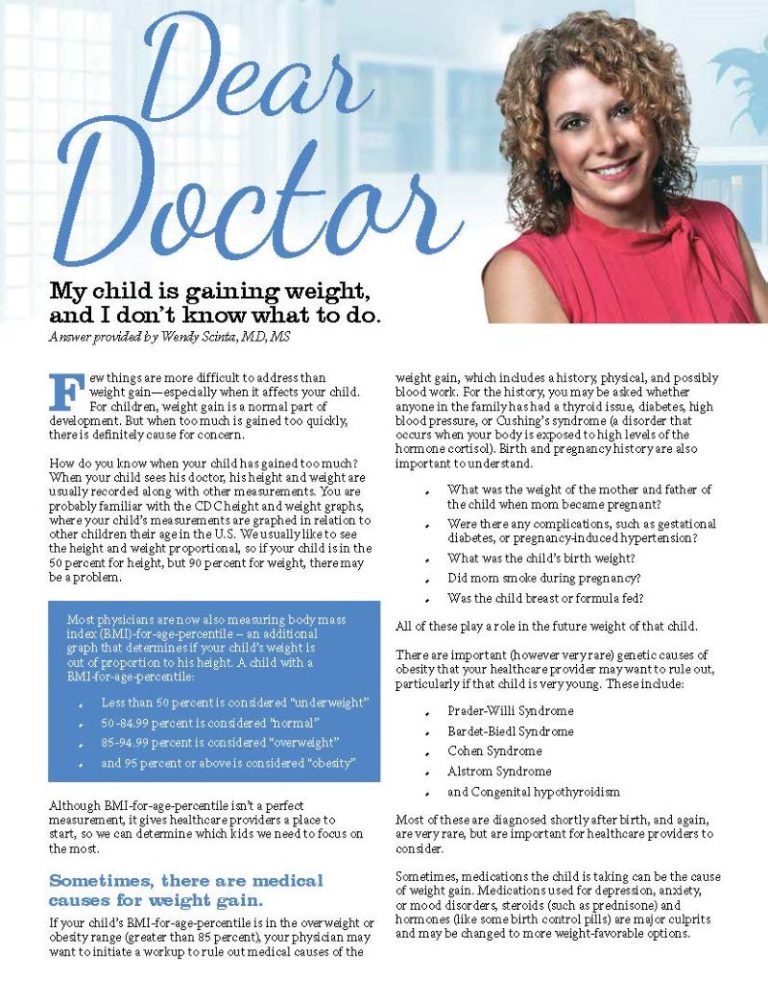
Answer provided by Wendy Scinta, MD, MS
Summer 2014
Few things are more difficult to address than weight gain—especially when it affects your child. For children, weight gain is a normal part of development. But when too much is gained too quickly, there is definitely cause for concern.
How do you know when your child has gained too much? When your child sees his doctor, his height and weight are usually recorded along with other measurements. You are probably familiar with the CDC height and weight graphs, where your child’s measurements are graphed in relation to other children their age in the U.S. We usually like to see the height and weight proportional, so if your child is in the 50 percent for height, but 90 percent for weight, there may be a problem.
Most physicians are now also measuring body mass index (BMI)-for-age-percentile – an additional graph that determines if your child’s weight is out of proportion to his height. A child with a BMI-for-age-percentile:
- Less than 50 percent is considered “underweight”
- 50-84.99 percent is considered “normal”
- 85-94.99 percent is considered “overweight”
- and 95 percent or above is considered “obesity”
Although BMI-for-age-percentile isn’t a perfect measurement, it gives healthcare providers a place to start, so we can determine which kids we need to focus on the most.
Sometimes, there are medical causes for weight gain.
If your child’s BMI-for-age-percentile is in the overweight or obesity range (greater than 85 percent), your physician may want to initiate a workup to rule out medical causes of the weight gain, which includes a history, physical, and possibly blood work. For the history, you may be asked whether anyone in the family has had a thyroid issue, diabetes, high blood pressure, or Cushing’s syndrome (a disorder that occurs when your body is exposed to high levels of the hormone cortisol). Birth and pregnancy history are also important to understand.
- What was the weight of the mother and father of the child when mom became pregnant?
- Were there any complications, such as gestational diabetes, or pregnancy-induced hypertension?
- What was the child’s birth weight?
- Did mom smoke during pregnancy?
- Was the child breast or formula-fed?
All of these play a role in the future weight of that child.
There are important (however very rare) genetic causes of obesity that your healthcare provider may want to rule out, particularly if that child is very young. These include:
- Prader-Willi Syndrome
- Bardet-Biedl Syndrome
- Cohen Syndrome
- Alstrom Syndrome
- and Congenital hypothyroidism
Most of these are diagnosed shortly after birth, and again, are very rare, but are important for healthcare providers to consider.
Sometimes, medications the child is taking can be the cause of weight gain. Medications used for depression, anxiety, or mood disorders, steroids (such as prednisone) and hormones (like some birth control pills) are major culprits and may be changed to more weight-favorable options.
What if there is no medical cause of the weight gain?
As an obesity medicine specialist, I can tell you that finding a true medical cause of obesity is quite rare. By and large, weight gain is the result of our “obesigenic” environment. That is: what we eat, when we eat, where we eat and how much. To a lesser extent, it is also related to how much we move in relation to our intake.
A shocking 1/3 of children in America struggle with a weight issue, and 2/3 of their parents fight the same battle. These numbers have tripled in the last 30 years, exploding when the “low-fat” diets came into play in the early 1980s. During this time, we decreased fat but increased carbohydrates in our diet – particularly sugar. Simultaneously, processed foods took over the grocery stores, and fast-food chains started to pop up on every street corner. For busy parents, these foods were affordable, convenient and tasty. Eventually, the homemade, sit-down family meal became a thing of the past. Today the average American family cooks and eats together at the dinner table only once per week.
When I am evaluating a child with a weight issue, I ask the child and caregiver some questions:
- Is the child eating breakfast?
- Do they bring their lunch or buy at school?
- Is dinner in the car, out at a restaurant or at home?
- Does the family prepare meals together and eat at the table?
Going without breakfast, frequent meals in the car or away from home and recurrent fast food intake all increase the chances that child will struggle with a weight problem.
How do you know if the extra weight is affecting your child’s health?
Unfortunately, it doesn’t take long for extra weight to affect other organs in the body. Sometimes, it is obvious, especially when the mass of the weight causes issues like pain in the knees, hips and even back. Children are vulnerable to some bone and joint issues that are unique for this age group: namely Slipped Capital Femoral Epiphysis (when the ball at the upper end of the femur or thigh bone slips backwards and causes pain in the hip or knee with an intermittent limp) and Blount’s disease (bowing of the tibia or shinbone). Severe headaches, particularly in the morning, can be due to a condition called Pseudotumor Cerebri or Idiopathic Intracranial Hypertension. Heavy snoring with witnessed apnea (cessation of breathing) can be signs of sleep apnea. A formal sleep study is often needed to confirm this diagnosis.
Other times, additional testing is needed to determine if unhealthy fat cells are causing metabolic changes in the body. These weight-related illnesses include:
- high blood pressure
- high cholesterol
- insulin resistance
- metabolic syndrome
- pre-diabetes
- diabetes
- gallstones
- kidney stones
- fatty-liver disease
- gastro-esophageal reflux
- nutritional deficiencies (such as vitamin D deficiency)
It is important to understand that the majority of these issues are not only treatable, but completely reversible with weight-loss.
Where do you go from here?
If the information in this article gives you cause for concern, visit your child’s pediatrician or family physician for a thorough workup. Your provider may decide to treat some issues immediately, or refer your child to an obesity medicine specialist or pediatric endocrinologist for further evaluation and treatment. In the meantime, there are changes you can make to immediately create a healthier environment for your family. Consider the following:
- Limit electronics time (Have them exercise for it!)
- Limit eating out to no more than once/week
- No electronics of any kind while eating (cell phones, computers, and television)
- Sit down to dinner as a family at least once/week
- Model good behavior (They are watching you!)
- Remove negative food queues (such as bowls of candy or bags of chips) and present positive ones (such as a big bowl of fruit)
- Downsize plates and bowls (our brain likes to fill space)
- Eat breakfast – that means everyone!
- Eliminate or strictly limit sugar-sweetened beverages
- Don’t give up on fruits and vegetables
For more information on my BOUNCE approach to treating childhood obesity, visit my site on the web at www.drwendydiet.com.
About the Author:
Dr. Wendy Scinta is an expert on adult and childhood obesity, and has successfully treated thousands of patients at her practice, Medical Weight Loss of New York, PLLC. She is the author of BOUNCE®, and has been featured by AMA News, CNN, MD News, the New York Times, Web MD, Women’s Health Magazine, Steve Harvey Show and more. Dr. Scinta is Vice President of the American Society of Bariatric Physicians, and was awarded their prestigious “Bariatrician of the Year” award at the Fall 2012 ASBP Obesity Conference. She is also a past member of the White House Task Force on Childhood Obesity.
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read Articleby Michelle “Shelly” Vicari Winter 2024 Winter has arrived! Don’t allow the chilly and damp weather to…
Read Articleby Kendall Griffey, OAC Communications Coordinator Winter 2024 The Obesity Action Coalition’s 12th annual Your Weight Matters…
Read Article