Dear Doctor: How Does Obesity Affect My Immune System?

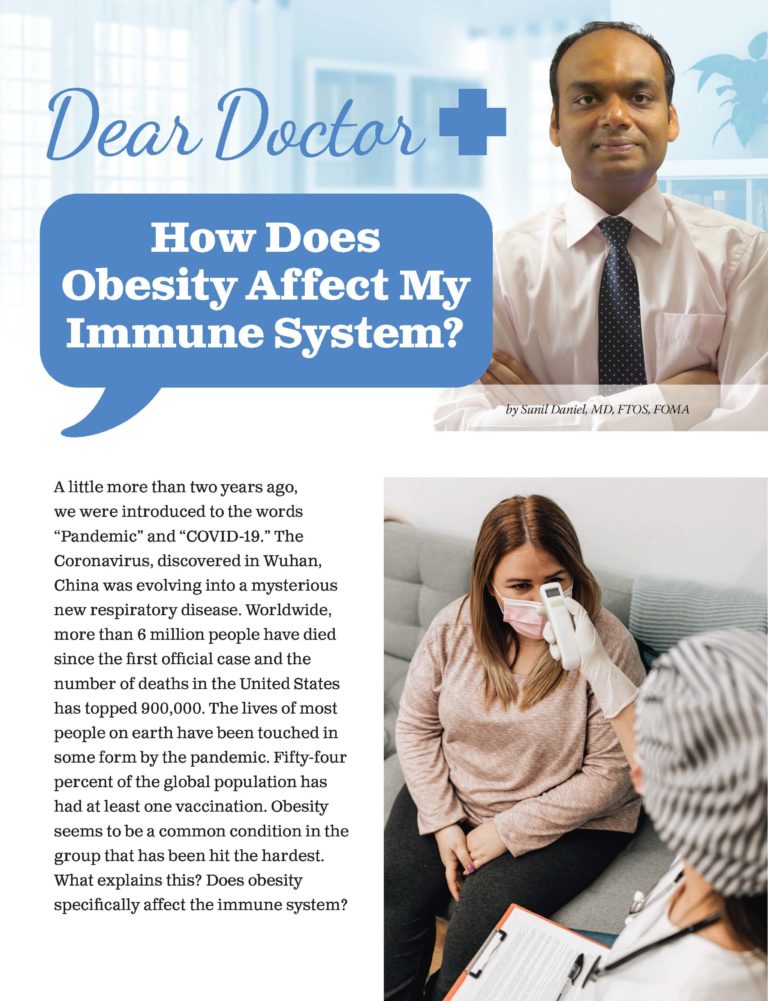
by Sunil Daniel, MD, FTOS, FOMA
Spring 2022
A little more than two years ago, we were introduced to the words “Pandemic” and “COVID-19.” The Coronavirus, discovered in Wuhan, China was evolving into a mysterious new respiratory disease. Worldwide, more than 6 million people have died since the first official case and the number of deaths in the United States has topped 900,000. The lives of most people on earth have been touched in some form by the pandemic. Fifty-four percent of the global population has had at least one vaccination. Obesity seems to be a common condition in the group that has been hit the hardest. What explains this? Does obesity specifically affect the immune system?
What Does the Immune System Do?
The immune system is a complex network of cells, tissues and organs. Together they help the body fight infections and other diseases. When germs such as bacteria or viruses invade the body, they attack and multiply. This is called an infection. The infection causes the disease that makes a person sick. Our immune system protects us from disease by fighting off germs.
Without an immune system, we would have no way to fight harmful substances that enter our body from the outside or harmful changes that occur inside. The main tasks of the immune system are:
- To fight disease-causing germs (pathogens) like bacteria, viruses, parasites or fungi, and remove them from the body
- To recognize and neutralize harmful substances from the environment
- To fight disease-causing changes in the body, such as cancer cells
The most important parts of our immune system are our skin, mucous membranes (the moist lining of organs and body cavities), white blood cells and the lymphatic system (thymus, spleen, tonsils, lymph nodes bone marrow, etc.).
How Does Obesity Affect the Immune System?
Obesity results in overreaction to infection and injury, causes the immune system to react even in the absence of infection and allows inflammation to continue even after recovery from injury or illness. This can lead to chronic inflammation, which is linked to various health conditions:
- Diabetes
- Heart disease
- Atherosclerosis – the buildup of fats, cholesterol and other substances in and on your artery walls
- Arthritis
- Sleep
- Cancer
Our immune system is divided into two parts:
- Innate immune system: This provides a general defense against harmful germs and substances that enter the body. This system is not very specific and mainly tries to kill or eat germs using cells such as “natural killer cells” and “phagocytes (eating cells).”
- Adaptive immune system: This is also known as a specific immune system. It makes antibodies which are made of proteins that help identify and neutralize a virus or bacteria. This system also has cells that are called “memory cells” that have an acquired (or learned) response. Because this system is constantly learning and adapting, the body can fight bacteria or viruses that change over time.
Antibodies Preventing Infection
Above, you can see an example from the National Institutes of Health (NIH) on how antibodies prevent infection from COVID-19.
Viral Infections and Obesity
Obesity is one of the most important conditions that make us vulnerable to viral infections. It changes the adaptive immune system in the following ways:
- Leptin – Leptin is a protein that is made in fat cells, circulates in the bloodstream and goes to the brain. It tells your brain that you have enough energy stored in your fat cells to engage in normal metabolic processes, thus inhibiting hunger. People with obesity may have resistance to leptin which can weaken their immune systems.
- Memory Cells – In obesity, memory cells in the immune system (CD4+ and CD8+ T cells) are reduced or depleted. These cells are essential to providing long-term immunity against viral functions. With fewer memory cells, the body must fight harder to provide immunity.
- The B-cell – Obesity leads to chronic low-grade inflammation which decreases the function of another important cell of the adaptive immune system: the B-cell. This cell is important in producing antibodies to fight viruses and bacteria.
Obesity is also a risk factor for the development of bacterial and fungal infections. Obesity disables the innate immune system which is the first line of defense against bacteria and fungi.
Conclusion
In summary, obesity stunts the immune system’s response to infections. One of the best ways to reduce the effects of excess weight and obesity on the body’s ability to fight infections is to see your healthcare provider and discuss weight management options.
About the Author:
Sunil Daniel, MD, FTOS, FOMA, is a board-certified obesity medicine physician with fellowship training in clinical nutrition and obesity management. He is a fellow of The Obesity Society and Obesity Medicine Association and has authored several scientific papers on obesity and its medical management. He is also an OAC National Board Member and serves on the Education Committee.
by Rachel Goldman, PhD, FTOS; Sarah Muntel, RD; and Stefanie Trilling Winter 2024 This section of Weight…
Read Articleby Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Articleby Kelli Richardson, RD You’ve probably heard the generic advice before: Eat your fruits and veggies. Limit…
Read Article