Dear Doctor: How Can I Manage My Weight While Taking Antidepressants?

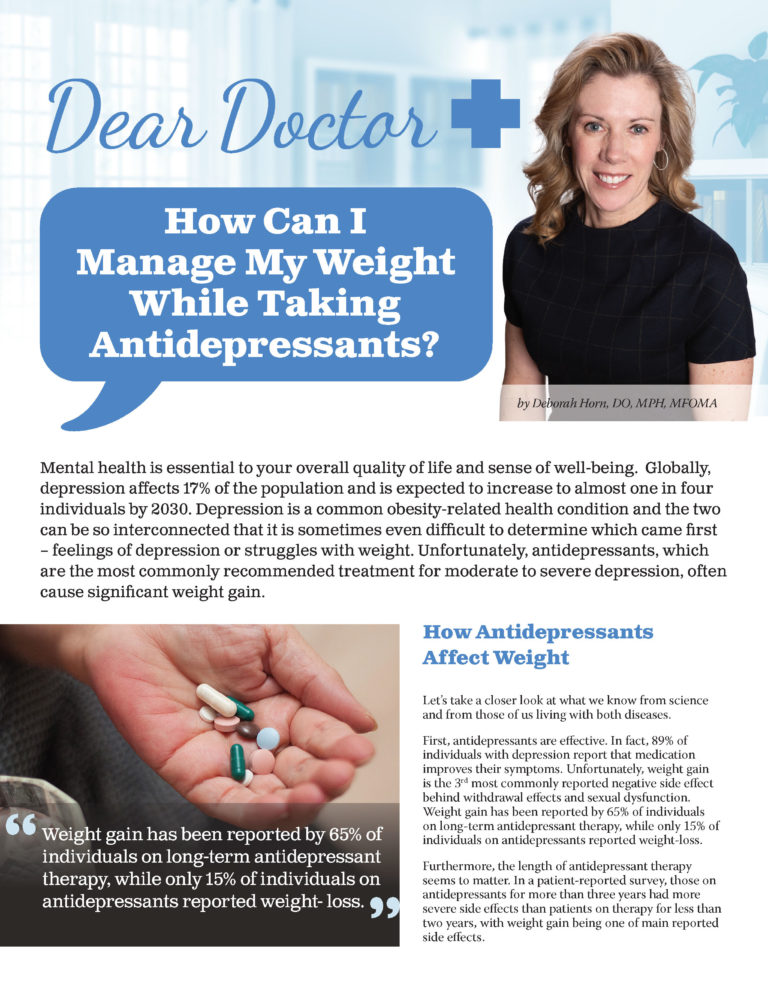
by Deborah Horn, DO, MPH, MFOMA
Summer 2021
Mental health is essential to your overall quality of life and sense of well-being. Globally, depression affects 17% of the population and is expected to increase to almost one in four individuals by 2030. Depression is a common obesity-related health condition and the two can be so interconnected that it is sometimes even difficult to determine which came first – feelings of depression or struggles with weight. Unfortunately, antidepressants, which are the most commonly recommended treatment for moderate to severe depression, often cause significant weight gain.
How Antidepressants Affect Weight
Let’s take a closer look at what we know from science and from those of us living with both diseases.
First, antidepressants are effective. In fact, 89% of individuals with depression report that medication improves their symptoms. Unfortunately, weight gain is the 3rd most commonly reported negative side effect behind withdrawal effects and sexual dysfunction. Weight gain has been reported by 65% of individuals on long-term antidepressant therapy, while only 15% of individuals on antidepressants reported weight-loss.
Furthermore, the length of antidepressant therapy seems to matter. In a patient-reported survey, those on antidepressants for more than three years had more severe side effects than patients on therapy for less than two years, with weight gain being one of main reported side effects.
Both changes in weight depend on the length of antidepressant therapy and choice of medication. Additionally, the body’s response to medication can change over time.
For example, let us consider a common class of antidepressants called selective serotonin reuptake inhibitors (SSRIs). This class includes medications that are used frequently like:
- Citalopram
- Paroxetine
- Sertraline
- Fluoxetine
They help with depression by blocking the reuptake of serotonin, a hormone in the brain that stabilizes our mood, feelings of well-being, and happiness. Serotonin levels are lower in people with depression and SSRIs help increase the amount of serotonin that is available to the brain. In the short-term, this increase in serotonin helps us feel full, decreases our food intake, and decreases our impulsiveness. But in the long-term, our body seems to adjust to these changes in stimulation. After 12 months of treatment, an SSRI can sometimes lead to weight gain due to cravings for carbohydrates and other potential factors.
Another factor that plays a role in weight while on antidepressants is whether or not you are struggling with obesity at the time the medication is initiated. For example, antidepressant medications that increase dopamine levels in the brain also affect energy balance. Individuals with obesity tend to have decreased dopamine, which is a chemical in the brain that influences mood as well as feelings of reward and motivation. Improving dopamine levels may help them lose weight. However, individuals without obesity may gain weight in response to an increase in dopamine signaling. This is a perfect example of how intertwined these two diseases can become as we try to improve one or both.
Optimizing Your Medication Choices
By following patients over time, we have been able to categorize antidepressants based on their risk of “drug-induced weight gain.” In the chart featured in this article, you will see that medications can be high, medium or low-risk.
When possible, it is beneficial to choose from medications that have a lower risk of weight gain. In fact, with the help of your physician or psychiatrist, you may find that you want to trying shifting to a lower-risk medication.
Whether you are starting an antidepressant or considering a change in your medication, please keep two important things in mind:
- First, the antidepressant needs to do its first job, which is to improve your depression symptoms.
- Second, your individual weight response to an antidepressant may be different from the most common responses which led to the categorization of the medication into a specific risk group.

Decreasing the Risk of Weight Gain
Here are four approaches we can lean towards to decrease the risk of weight gain on antidepressants.
- Recognize that finding the right antidepressant may take time. Many patients report that it can take a trial of several different antidepressants to determine the one that works best for their depression and has the least side effects. This is where individualized precision medicine and commitment by both you and your healthcare provider are essential.
- Monitor your weight for changes. It sounds obvious, but this simple approach is key to identifying and correcting medication-driven changes in your weight. Weight gain on antidepressants can occur in the first few months on therapy and lead to stopping medication. It can also occur after a year or more of antidepressant therapy due to changes in the long-term response from the body.
- Combine medication with therapy. Counseling can be a key component to successful depression treatment. Counseling can provide you with an opportunity to talk about your weight journey, food relationships, and work towards solutions to barriers that might be holding you back in both your mental and physical health.
- Stay active. Physical activity has been shown to be effective in the treatment of depression and obesity. In some individuals, regular physical activity has been as effective as medication for the treatment of mild to moderate depression that has been previously well-controlled on single antidepressants. It may also help decrease the number of antidepressants needed or decrease the dose required to control symptoms.
Conclusion
In summary, there are many pieces to the puzzle when it comes to treating obesity while also taking antidepressants. The journey must be individualized. If depression and obesity are two areas that you are working on as you strive to improve your health, then it is time to map out your plan. You know your body best, so always be sure to tell your healthcare provider about any struggles you may be having with depression or weight gain. You can work together to develop a plan that meets your mental and physical needs.
About the Author:
Deborah Horn, DO, MPH, MFOMA, is the President of the Obesity Medicine Association and Clinical Assistant Professor in the Department of Surgery at The University of Texas McGovern Medical School at Houston. She is the Medical Director for the UTHealth Center for Obesity Medicine and Metabolic Performance. Dr. Horn was also the recipient of the Obesity Action Coalition’s (OAC) Healthcare Provider Advocate of the Year award – an award given to a healthcare provider who is a tireless advocate for patients, the OAC and the cause of obesity.
by Robyn Pashby, PhD Winter 2024 “No one is ever going to date you if you don’t…
Read Articleby Leslie M. Golden, MD, MPH, ABOM Diplomate Winter 2024 The journey to overcoming obesity is a…
Read ArticleDid you know that stress can have an impact on weight? Many people increase their food intake…
View Video