Dear Doctor – Can weight-loss surgery affect my vision?

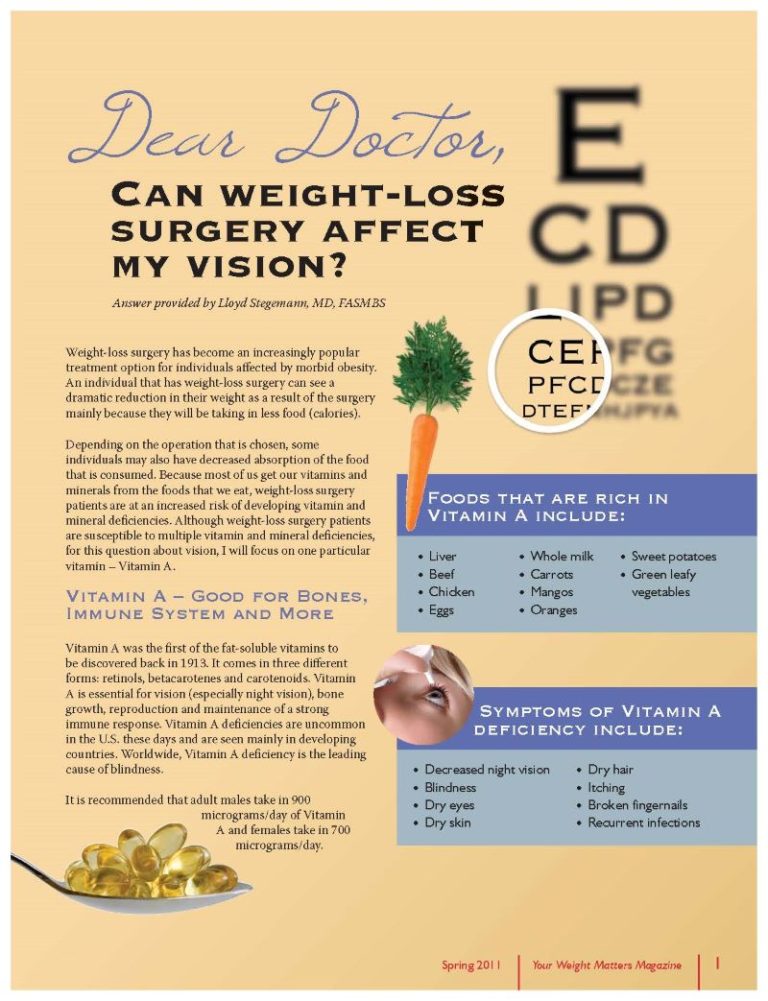
Answer provided by Lloyd Stegemann, MD, FASMBS
Spring 2011
Weight-loss surgery has become an increasingly popular treatment option for individuals affected by morbid obesity. An individual that has weight-loss surgery can see a dramatic reduction in their weight as a result of the surgery mainly because they will be taking in less food (calories).
Depending on the operation that is chosen, some individuals may also have decreased absorption of the food that is consumed. Because most of us get our vitamins and minerals from the foods that we eat, weight-loss surgery patients are at an increased risk of developing vitamin and mineral deficiencies.
Although weight-loss surgery patients are susceptible to multiple vitamin and mineral deficiencies, for this question about vision, I will focus on one particular vitamin – Vitamin A.
Vitamin A – Good for Bones, Immune System and More
Vitamin A was the first of the fat-soluble vitamins to be discovered back in 1913. It comes in three different forms: retinols, betacarotenes and carotenoids. Vitamin A is essential for vision (especially night vision), bone growth, reproduction and maintenance of a strong immune response. Vitamin A deficiencies are uncommon in the U.S. these days and are seen mainly in developing countries. Worldwide, Vitamin A deficiency is the leading cause of blindness.
It is recommended that adult males take in 900 micrograms/day of Vitamin A and females take in 700 micrograms/day.
Foods that are rich in Vitamin A include:
– Liver
– Beef
– Chicken
– Eggs
– Whole milk
– Carrots
– Mangos
– Oranges
– Sweet potatoes
– Green leafy vegetables
Symptoms of Vitamin A deficiency include:
– Decreased night vision
– Blindness
– Dry eyes
– Dry skin
– Dry hair
– Itching
– Broken fingernails
– Recurrent infections
Weight-loss Surgery and Vitamin A Deficiency
The incidence of Vitamin A deficiencies after weight-loss surgery is unclear. What is clear is that the incidence of Vitamin A deficiency increases depending on the operation performed. There is very little literature on the incidence of Vitamin A deficiencies with adjustable gastric band patients, but it is thought to be quite low.
The bulk of the literature on Vitamin A deficiencies after weight-loss surgery focuses on the stapled procedures (gastric bypass and biliopancreatic diversion). The reported incidence of Vitamin A deficiencies one year after gastric bypass is 10 to 30 percent and upwards of 50 to 60 percent after biliopancreatic diversion. It is recommended that gastric bypass and biliopancreatic diversion patients take at least 10,000 international units of Vitamin A daily and probably more importantly have their Vitamin A levels checked on a regular basis.
Unlike Vitamin B12, it is possible to take too much Vitamin A. Symptoms of over-supplementation of Vitamin A include gastrointestinal complaints, irritability, altered mental status, blurry vision and weakness. It is critically important that any female weight-loss surgery patient that is contemplating a pregnancy be assured that their Vitamin A levels are normal before and during the pregnancy. There are several case reports of newborns having vision problems if their mother is Vitamin A deficient during the pregnancy.
Vitamin A deficiencies after weight-loss surgery are not uncommon. These deficiencies can have detrimental effects on vision and the immune system. It is important that any individual that has had weight-loss surgery take the recommended dose of vitamins and minerals and follow-up with their program on a regular basis to prevent long-term complications from vitamin and mineral deficiencies.
Answer provided by:
Lloyd Stegemann, MD, FASMBS, is a private practice bariatric surgeon in San Antonio. He is the driving force behind the Texas Weight Loss Surgery Summit and the formation of the Texas Association of Bariatric Surgeons. Dr. Stegemann is a member of the American Society for Metabolic and Bariatric Surgery and the OAC National Board of Directors.
by OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Article