BMI: The Good, The Bad, and The Ugly.

by David Edelson, MD
Winter 2012
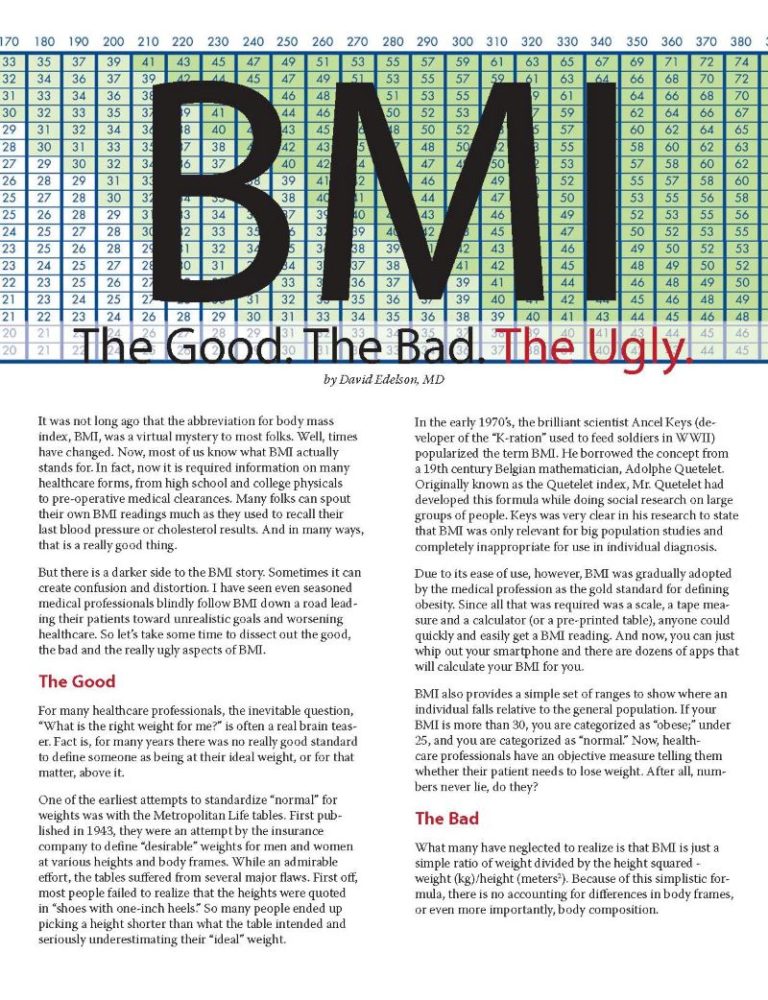
It was not long ago that the abbreviation for body mass index, BMI, was a virtual mystery to most folks. Well, times have changed. Now, most of us know what BMI actually stands for. In fact, now it is required information on many healthcare forms, from high school and college physicals to pre-operative medical clearances. Many folks can spout their own BMI readings much as they used to recall their last blood pressure or cholesterol results. And in many ways, that is a really good thing.
But there is a darker side to the BMI story. Sometimes it can create confusion and distortion. I have seen even seasoned medical professionals blindly follow BMI down a road leading their patients toward unrealistic goals and worsening healthcare. So, let’s take some time to dissect out the good, the bad and the really ugly aspects of BMI.
The Good
For many healthcare professionals, the inevitable question, “What is the right weight for me?” is often a real brain teaser. Fact is, for many years there was no really good standard to define someone as being at their ideal weight, or for that matter, above it.
One of the earliest attempts to standardize “normal” for weights was with the Metropolitan Life tables. First published in 1943, they were an attempt by the insurance company to define “desirable” weights for men and women at various heights and body frames. While an admirable effort, the tables suffered from several major flaws. First off, most people failed to realize that the heights were quoted in “shoes with one-inch heels.” So many people ended up picking a height shorter than what the table intended and seriously underestimating their “ideal” weight.
In the early 1970’s, the brilliant scientist Ancel Keys (developer of the “K-ration” used to feed soldiers in WWII) popularized the term BMI. He borrowed the concept from a 19th century Belgian mathematician, Adolphe Quetelet. Originally known as the Quetelet index, Mr. Quetelet had developed this formula while doing social research on large groups of people. Keys was very clear in his research to state that BMI was only relevant for big population studies and completely inappropriate for use in individual diagnosis.
Due to its ease of use, however, BMI was gradually adopted by the medical profession as the gold standard for defining obesity. Since all that was required was a scale, a tape measure and a calculator (or a pre-printed table), anyone could quickly and easily get a BMI reading. And now, you can just whip out your smartphone and there are dozens of apps that will calculate your BMI for you.
BMI also provides a simple set of ranges to show where an individual falls relative to the general population. If your BMI is more than 30, you are categorized as having severe obesity; under 25, and you are categorized as “normal.” Now, healthcare professionals have an objective measure telling them whether their patient needs to lose weight. After all, numbers never lie, do they?
The Bad
What many have neglected to realize is that BMI is just a simple ratio of weight divided by the height squared – weight (kg)/height (meters2). Because of this simplistic formula, there is no accounting for differences in body frames, or even more importantly, body composition.
My favorite example of this is a quiz I have given many times, including to physicians at medical grand rounds at some of the top teaching hospitals in the country. I like to give it in the form of a “Jeopardy Challenge,” with the category being “Severe Obesity, or Not Severe Obesity.” So with all due respect to Alex Trebek, the answer is:
“This famous ex-politician and former actor recently measured in at 6’ 2” tall and 257 pounds, with a calculated BMI of 33.0.”
When asked to respond, 100 percent of doctors answered “Severe Obesity!” Yet, when the next slide showed former California Governor Arnold Schwarzenegger, in his prime body building days, playing his role as Conan the Barbarian, the problem becomes clear. How could someone in that kind of shape have a BMI well above 30?
The real answer: muscle is heavier than fat!
BMI tells you nothing about what that individual’s body is made up of. Someone that is in superb condition, with lots of lean muscle, could be the same weight or even heavier than someone else at the same height, but in terrible shape. Our friend Arnold might have had a BMI of 33, but his body fat percentage was around 7 percent. For comparison, an average male would expect to have between 12 percent and 22 percent body fat.
So, now the problem begins to come into focus. BMI, while being a reasonable estimator of obesity in someone of average conditioning, becomes a terrible predictor in people with either lots of lean muscle (trained athletes) or very little lean muscle (severely de-conditioned individuals). BMI does not tell you anything about what is going on inside someone’s body, which is what we ALL should really be interested in.
BMI may actually be under-estimating the rates of obesity in this country. A study in 2008 by Romero-Corral et al. examined data from the United States Third National Health and Nutrition Examination Survey (NHANES III) and discovered that using BMI alone, 21 percent of men and 31 percent of women met the criteria for being affected by obesity. But, when they went back and looked at body fat percentages (the ratio of body fat to total body weight), the rates skyrocketed to 50 percent of men and 62 percent of women.
The Ugly
So why is this a problem? Well, first of all, many big institutions use BMI to determine your risk for health problems. The most obvious ones are within the insurance industry. Just go try to get a life insurance policy or disability insurance with a BMI more than 30 and see what happens. The bean counters figure that if you are affected by obesity, you are high-risk. So, they hedge their bets by raising the premium you will pay for the same amount of coverage, as opposed to someone with a normal BMI. Worse yet, they might even refuse to give you a policy altogether. So in theory, you could be an elite Olympic athlete in the best shape of your career and have some insurance representative telling you that you do not qualify for coverage. But, it gets even worse.
Furthermore, studies are now finding that BMI is a very poor predictor of who might be at risk of developing heart disease. A study at the Centers for Disease Control (CDC) by Flegal-Graubard, et.al., published in JAMA in 2005 seemed to indicate that overweight individuals (BMI 25 to 30) did not have any increased risk of death compared to normal weight individuals (BMI under 25); however no effort was made to see what the body fat levels of these people were.
As someone who works out regularly, has a BMI of 28, but a body fat percentage level at a respectable 12 percent, I would argue that studies like this that just use BMI do a great disservice to the medical community and the population at large. It may also give individuals in poor shape, but only mildly overweight, the impression that they can continue their current poor lifestyles with little or no risk. Bad idea.
The Alternatives
Certainly no sane healthcare professional would tell you that we use some objective standard to say who needs to lose weight. Most importantly, we need to know precisely who is at risk for health problems related to their weight. I’m just here to tell you that BMI is not perfect.
Fortunately, there are several excellent alternative measurements available right now that we CAN use:
Body Fat Percentage (BF%):
In my opinion, this should be the gold standard for judging obesity. It is simply the ratio of the amount of fat in your body divided by your total body weight. There are many methods to determine body fat percentage, from simple skin fold calipers costing a few dollars to more advanced machines costing thousands.
But recently, bioimpedence scales have become a simple, relatively accurate way to measure body fat percentage. They take measurements by sending a small electric current through the body. These scales are available for under $100 and can measure body fat percentage quickly and easily right in your own home. While professional models may be more expensive, there really is no excuse for any clinician dealing with obesity to not have one.
With the understanding that these devices should NEVER be used if you are pregnant or have a pacemaker/defibrillator device, they are simple and elegant tools that can help clinicians establish healthy and realistic parameters for healthy weight.
Here are tables developed by the World Health Organization (WHO) and National Institutes of Health (NIH) providing reference ranges for body fat percentage:
WOMEN
| Age | Underfat | Healthy Range | Overweight | Severe Obesity |
| 20-40 yrs | Under 21% | 21-33% | 33-39% | Over 39% |
| 41-60 yrs | Under 23% | 23-35% | 35-40% | Over 40% |
| 61-79 yrs | Under 24% | 24-36% | 36-42% | Over 42% |
MEN
| Age | Underfat | Healthy Range | Overweight | Severe Obesity |
| 20-40 yrs | Under 8% | 8-19% | 19-25% | Over 25% |
| 41-60 yrs | Under 11% | 11-22% | 22-27% | Over 27% |
| 61-79 yrs | Under 13% | 13-25% | 25-30% | Over 30% |
Waist Measurements:
If you do not have a body fat scale, there is a backup plan: a simple tape measure. For about $1.99, anyone can learn if they really need to lose weight to improve their health. There are three ways to use this amazing piece of low-tech technology:
- Waist- to-height Ratio (WHtR): A recent study by Scneider-Friedrich, et. al. in the Journal of Clinical Endocrinology & Metabolism showed WHtR to be the best predictor of cardiovascular risk and mortality. They also showed BMI to be a terrible predictor and strongly discouraged its use. In general, men should have a WHtR less than 0.55 and women less than 0.53. For those over the age of 50, the number should be below 0.60.
- Waist-to-hip Ratio (WHR): By comparing the smallest measurement around your waist (near the belly button) to the largest around your hips, you are getting great information about belly fat. The fat, also known as mesenteric fat, seems to be the culprit for much of the health risks related to being overweight. A ratio more than 0.8 for women and 0.95 for men indicates too much fat.
- Waist Circumference (WC): While the simplest measure, it still has some powerful advocates. This number is used by the American Heart Association as one of the critical pieces of information for determining metabolic syndrome, a pre-diabetic condition. Men with waist measurements greater than 40 inches and women more than 35 inches should speak to a healthcare professional about their weight.
Conclusion
As an obesity medicine specialist, I applaud the medical community’s attempts to begin serious efforts to screen our patients for problems with their weight. However, I strongly discourage relying solely on BMI to make that determination. As professionals, we need to start understanding the complexity of the serious, chronic disease we currently call obesity. I have no objection to BMI as a simple screening tool; however, I implore my colleagues to start looking at body fat percentage or waist-to-height ratios on every patient we see. Only then can we begin to focus our best efforts on the patients that need our help the most.
About the Author:
David Edelson, MD, is a graduate of Northwestern University’s six-year honor’s program in medical education and is board certified in both internal medicine and bariatric medicine. A two-time winner of the Faculty Teaching Award, Dr. Edelson is an assistant clinical professor of medicine at Albert Einstein College of Medicine. In 2000, he founded HealthBridge, an integrated healthcare facility specializing in obesity medicine.
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read ArticleTelemedicine became a popular tool during the pandemic because it allows healthcare professionals to provide medical care…
View Videoby Kendall Griffey, OAC Staff; and Chrystal Jones, OAC Staff Fall 2022 For over ten years, the…
Read Article