A Patient’s Guide to Advocating for Improved Access to Weight-Loss Surgery under Medicare

The Importance of Advocacy
Advocacy is defined as the act of pleading or arguing in favor of something, such as a cause, idea or policy. Advocacy comes in many forms. This guide will specifically highlight how to effectively work with the Centers for Medicare & Medicaid Services (CMS), the government agency that oversees Medicare.
Regulatory officials at the local, state and federal level play a significant role in our society and healthcare. Often, the laws they administer directly influence our day-to-day lives or regulate the medical treatments we receive. However, the majority of regulatory officials know little about obesity, its effects and treatments. The OAC seeks to increase awareness among regulatory officials by encouraging patients affected by obesity to become advocates.
As an American, it is your right to build relationships with government officials and to advocate for positive change. It is through the voice of patients, family members and medical professionals that officials learn how current, pending and future laws and regulations impact Americans with obesity. The OAC encourages you to become an advocate for change.
Accessing Weight-Loss Surgery under Medicare
On November 23, 2005, CMS, the governing agency of Medicare, released proposed new rules under a National Coverage Decision (NCD) for weight-loss surgery. The OAC strongly believes these proposed rules are a positive change that will improve access to the treatment of morbid obesity. Understanding the rules and regulations proposed under the NCD are important not only for those currently insured by Medicare but also for those covered by commercial insurance policies as many insurance companies base their coverage decisions on Medicare’s policies.
The proposed rules validate the treatment of morbid obesity through weight-loss surgery. Surgical treatment options for Medicare recipients, who are under the age of 65, will now include both open and laparoscopic roux-en-y gastric bypass as well as laparoscopic adjustable gastric banding (commonly known at Lap-Band) as long as the patient has a body mass index (BMI) of 35 or greater, one obesity-related health problem and has been previously unsuccessful with the medical treatment of their obesity. The OAC strongly supports the coverage of weight-loss surgery as studies show the surgical treatment of morbid obesity decreases mortality, improves or resolves obesity-related illnesses and improves quality of life.
However, the OAC does have specific concerns with portions of the NCD as it proposes eliminating coverage of weight-loss surgery as a benefit for those over the age of 65. Other concerns include not specifying or defining the requirement of being unsuccessful with the medical treatment of obesity to access surgery, failure to provide coverage of biliopancreatic diversion (BPD) and duooudenal switch (DS) and a lack of information on payment for the required future follow-up physician and healthcare professional visits required for optimal post-operative care.
Medicare Recipients 65 and Older
In the NCD, CMS specifically cites data from a recent study citing elevated risk for older patients by David Flum, MD as their reason for non-coverage of those 65 an older. However, Dr. Flum does point out in his study, and in his own comments to CMS, that the risks of weight-loss surgery among those 65 and older were similar to younger patients when performed by experienced surgeons. As such, the OAC is proposing and encouraging our fellow patients to support that Medicare cover surgery for those more than 65 years of age under Medicare’s Coverage with Evidence Determination (CED) program with the conditions that surgeons be appropriately experienced (granted status as a American Society of Bariatric Surgeons’ Centers of Excellence Program or similarly developed future programs) and that mortality and complication data be collected to evaluate the potential of a future expansion of coverage.
Previous Unsuccessful Medical Treatment
The NCD mentions a requirement of previous unsuccessful medical treatment of obesity, but does not apply specific definitions or requirements. As there is no clinical evidence that such programs improve the outcomes of weight-loss surgery and as requirements can vary widely from commercial based insurers, the OAC requests that Medicare adopt a policy of three to six months of medically supervised (physician, allied health professional or commercial agency) weight-loss during the past five years but not necessarily within one year of surgery.
BPD and DS
Although not as common as gastric bypass and Lap-Band procedures, BPD and DS may be the preferred surgery types of for some patients. The OAC believes that a patient and their surgeon are best able to make the appropriate decision in their surgery options. As such, the OAC is also proposing that Medicare’s CED program be utilized to allow for coverage of BPD and DS under similar circumstances to the 65 and older population – a requirement for appropriately experienced surgeons and data collection for comparative studies to other types of weight-loss surgery.
Payment of Follow-Up Visits
As part of the OAC’s belief that comprehensive long-term follow-up care is required to be a successful weight-loss surgery patient, the OAC is concerned that follow-up physician and healthcare professional visits are not discussed in the NCD. Such visits could include follow-up consultations with a surgeon and/or dietitian and in the case of Lap-Band patients, required fills to assure their band is working effectively. The OAC calls on Medicare to adopt policies to allow for coverage of medically-necessary follow-up care.
Call-to-Action
The OAC requests that you send your own comments to Medicare on the NCD. Feel free to share your own thoughts on the NCD or echo the OAC’s thanking Medicare for proposing improved access to weight-loss surgery and asking for the revisions detailed above. This issue is very important as many commercial insurance companies follow Medicare’s lead in developing their own policies.
What Can You Do to Advocate?
Anyone can be an advocate. Here are a few suggestions on what you can do.
- Share this information with family, friends and support groups and encourage them to get involved. The more individuals involved, the stronger our voice. Feel free to make copies of this guide or call the OAC National Office at (800) 717-3117 for additional copies.
- Post Send a comment on the National Coverage Decision to CMS by accessing the CMS Web site (see below).
- Keep the OAC informed of your actions. Did you post send a comment to CMS? Did you post a link to this guide on your Online support group? Let us know by mailing or e-mailing us a copy of your letter or message.
How Do I Comment to CMS?
CMS will be accepting comments on the National Coverage Decision until December 23, 2005. To comment, click here.
To send your comments by fax, submit them to:
(410) 786-9286 – Attention: Katherine Tillman
Looking for Tips on What to Write?
Below, please find some suggested topics, facts, do’s, don’ts and a sample letter.
- If you are a post-weight loss surgery patient, please share in your comment the difference your weight-loss has made in your life from both a quality of life and health standpoint. For instance, if you are no longer a diabetic, you now take a reduced number of medications and/or no longer suffer from sleep apnea. Your personal story is powerful.
- Please include if you were Medicare eligible when you received your surgery, if Medicare paid for the operation and your age at surgery.
- If you are seeking weight-loss surgery, explain your personal preparation, what health complications you are currently experiencing, how they affect your quality of life and the relief or burden placed on you by the new policies created by the National Coverage Decision.
- If you are a family member or friend of a weight-loss surgery patient, detail the difference weight-loss has made in your family member/friend’s life or how much they would benefit from receiving these services.
Facts about Bariatric (Weight-Loss) Surgery
- Extends the lives of patients
- Causes significant weight-loss
- Decreases the incidence and costs of obesity-related diseases, such as diabetes, hypertension, cancers and heart disease
- Improves the quality of life of the recipients
- For more facts, see the OAC publication, “Fact Sheet: Why it makes sense to provide treatment for obesity through bariatric surgery”
Do’s
- Write legibly and be brief and to the point. Short comments are the most effective.
- Thank CMS for their efforts to expand access to bariatric surgery.
- Give your reasons for supporting the proposed National Coverage Decision and raise any concerns.
- Be courteous and reasonable.
- Include all of your contact information.
- Double check your information for accuracy.
- Use correct grammar and complete sentences.
- Use a spell check feature.
- Include your personal story.
Don’ts
- Try not to be longwinded.
- Avoid a righteous tone.
- Avoid abbreviations.
- Do not threaten anyone.
- Do not demand anything from the individual.
- Do not refer or allude to politics or government as sleazy or dishonorable.
Sample Comment
Below, please find a sample letter that will help you get started:
In your first paragraph, mention the following points:
1. Thank CMS for their efforts to improve access to weight-loss surgery through a National Coverage Decision. Highlight any positives or negatives you may have with the decision at this point.
2. Discuss how this specific issue affects you and your family.
In your second paragraph, mention the following items:
1. Further elaborate how the issue affects or has affected you.
2. Share your personal connection with the issue in question. (Remember to remain brief. A short comment can accomplish just as much as a long one.)
In your last paragraph, discuss the following closing items:
1. Urge them to continue their efforts to expand the treatment of morbid obesity.
Sincerely,
Your Full Name
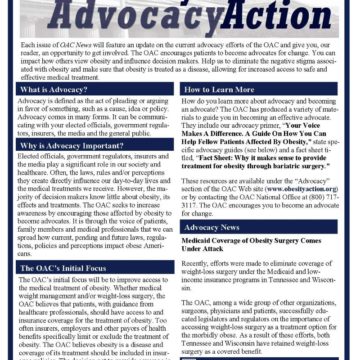
by Chrystal Jones, OAC Advocacy Manager Spring 2024 The Obesity Action Coalition (OAC) is the only patient-focused…
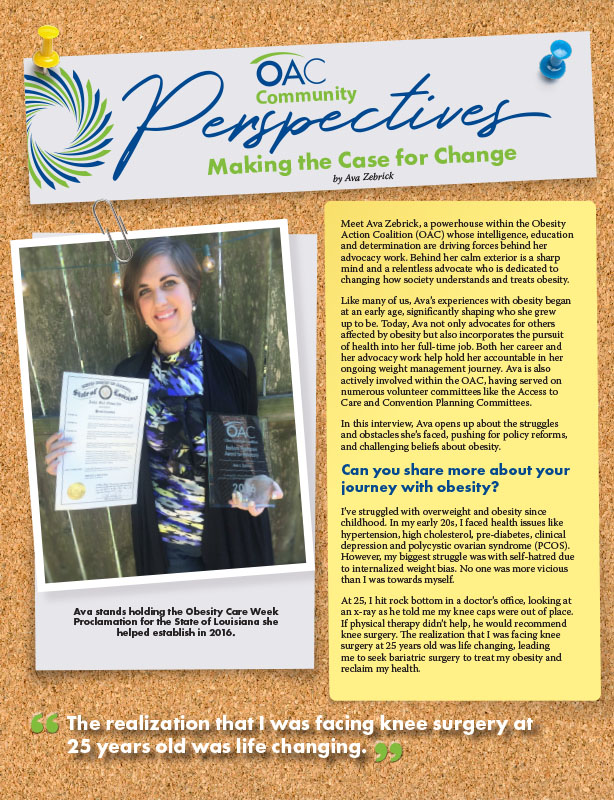
Read Articleby Ava Zebrick Spring 2024 Meet Ava Zebrick, a powerhouse within the Obesity Action Coalition (OAC) whose…
Read ArticleThe OAC is honored to welcome three new members to the OAC National Board of Directors. Jason Krynicki,…
Read Article