What is dumping, and why am I experiencing it?

by Taghreed Almahmeed, MD, FRCSC, and Michel Murr, MD, FACS
Spring 2006
Dumping syndrome is a group of symptoms caused by rapid passage of undigested food into the small intestine. The stomach has a valve at the top and bottom, and serves as an acid-filled storage tank, breaking food intake down into small, component parts and passing it to the small bowel in small increments.
After gastric bypass, ingested food passes directly into the small bowel, mixed only with saliva, but not the stomach acid. The component parts of the undigested food remain fairly intact and therefore large.
The small intestine responds by diluting the ingested food through a process of “water recruitment.” The “richer” the food, in terms of sugar content, the more water will rush into the small intestine to dilute it. This is referred to as “early dumping.”
Early Dumping and Late Dumping
Early dumping occurs a few minutes to 45 minutes after eating. Symptoms are not life-threatening, but can be frightening to the unsuspecting patient. Symptoms of early dumping are:
- Weakness and fainting
- Sweating
- Irregular and rapid heartbeat
- Low blood pressure
- Flushing of the skin
- Dizziness
- Shortness of breath
- Vomiting
- Diarrhea and cramps
Late dumping occurs two to three hours after eating. It is caused by excess insulin produced in response to rapid entry of food and fluids into the small intestine. The high insulin levels lower low blood glucose level and cause symptoms including:
- Perspiration
- Hunger
- Shakiness
- Anxiety
- Difficulty to concentrate
- Exhaustion
- Faintness
The diagnosis of late dumping syndrome can often be confirmed through frequent blood sampling to measure blood glucose.
You can prevent early and late dumping by avoiding the foods that cause dumping. In other words – sugars, starches and fried foods. Eat at least five to six small, evenly spaced meals a day. Take meals dry (i.e. without water or beverages, and drink fluids only between meals). Because carbohydrate intake is restricted, protein and fat intake should be increased to fulfill energy needs. Examples include meats, cheeses, eggs, nuts, toast, potatoes and rice crackers. Milk and milk products are generally not tolerated and should be avoided.
Each person has a different tolerance, and you will discover what your personal safe foods might be throughout your post surgery life. Person “A” might have no problem with strawberries and person “B” might experience dumping every time a few strawberries are eaten and person “C” might be able to eat strawberries only if they are a little unripe. You will learn what your own trigger foods might be. Be aware that these may change over time as your bypass matures.
General Measures to Treat Dumping
For early dumping, lie down for 45 minutes until symptoms pass to minimize the chances of fainting. For late dumping, eat small amounts of sugar candy or drink sweetened juice until the symptoms of low blood sugar resolve. Additionally you can supplement food with dietary fibers such as fruit, vegetables and grain products. Many medical therapies have been tested, including pectin, guar gum and glucomannan. These dietary fibers form gels with carbohydrates, resulting in delayed glucose absorption and therefore avoiding a sharp increase in insulin. However in 3 to 5 percent of instances, severe symptoms of dumping can continue despite dietary changes. This results in marked weight-loss, fear of eating and outdoor activities, or even an inability to maintain full time employment.
Medical management of dumping includes acarbose or octreotide. Acarbose delays absorption of food and maintains an even blood glucose level. Octreotide is an analog of a hormone in the digestive system that can alleviate dumping by inhibiting insulin release and by slowing transit of food in the small intestine.
Dumping is Common
Dumping syndrome is a common post-surgical complication after gastric surgery. The symptoms of dumping may cause considerable morbidity. If medical management fails to provide adequate symptom relief, remedial surgery should be offered with the understanding that even surgical intervention may not be successful. Normally most patients have a spontaneous recovery as the digestive system adapts after surgery. Early dumping syndrome usually occurs for three to four months after surgery. Late dumping syndrome can occur for an entire year, but may persist for many years. If you experience any of these symptoms, contact your health provider to review your food diary and implement changes to help you.
About the Authors:
Taghreed Almahmeed, MD, FRCSC, is currently an Advanced Laparoscopic and Bariatric Surgery Clinical Fellow at Tampa General Hospital. She completed her training in general surgery at the University of British Columbia in Vancouver, British Columbia, Canada.
Michel Murr, MD, FACS, is an Associate Professor of Surgery at the University of South Florida and a leading authority in bariatric surgery nationwide. He pioneered laparoscopic gastric bypass in the Tampa Bay area and has done extensive research on obesity and its surgical treatment. His comprehensive multi-disciplinary bariatric team performs more than 300 surgeries yearly.
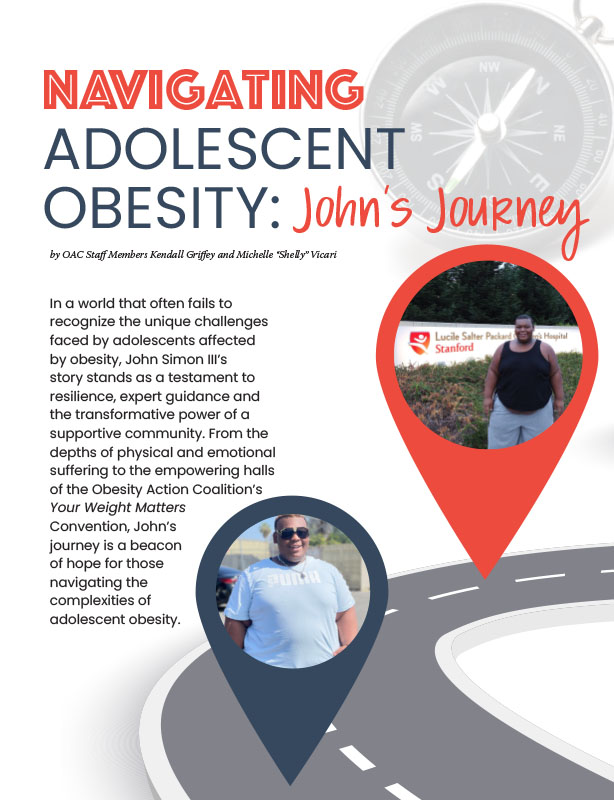
by OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read ArticlePost-operative addiction is often overly simplified as transfer addiction or cross-addiction, assuming individuals “trade” compulsive eating for…
View Video