The Future of Telehealth in Obesity Care

by Florencia Halperin, MD, MMSc
Winter 2022
The use of telehealth increased exponentially during the beginning of the COVID-19 crisis. Telehealth visits were up 154% in late March 2020 compared to the previous year, according to the Centers for Disease Control (CDC). Since then, patients and clinicians alike believe the increased use of telehealth services is here to stay.
What is Telehealth and How Does it Relate to Obesity?
Telehealth specifically refers to the use of live video conferencing to provide clinical services, much like a traditional one-on-one visit in the office, but online. During the pandemic, primary care and specialty providers used telehealth to address almost all aspects of care. However, telehealth may be particularly well-suited to address certain medical conditions such as obesity. Continuing to leverage telehealth has the potential to transform the future of obesity care.
Obesity is a vastly undertreated chronic disease. More than 40% of the U.S. population lives with obesity, but less than 1% receives medical treatment. Access to medical care to address obesity is generally limited, with less than 5,000 doctors who are accredited by the American Board of Obesity Medicine (ABOM) in the entire country, most of them practicing in urban areas.
Telehealth has made it easier to connect with these physicians for those living in more distant geographic regions or for those with difficulty making the trip to an in-person clinic. Telehealth has also expanded access to a multi-disciplinary team, making it more convenient to work with Registered Dietitians, professional exercise specialists, mental health professionals, or others who address important aspects of an individual’s needs.
How Can Telehealth Help Those Living with Obesity?
Incorporating telehealth into weight management may also be important for lowering the cost of care. Eliminating travel often reduces the immediate cost of visits to a patient, and using telehealth is generally considered to be more cost-effective. Many states have implemented ‘parity’ regulations that require insurance companies to cover telemedicine visits the same way they cover in-person visits.
Telehealth also brings a degree of privacy and comfort that some people living with obesity may appreciate. Bias, shame and stigma are common barriers to obtaining health care for individuals with obesity, and these are often a reality even within medical settings. A specialized obesity care team should provide empathetic and judgment-free care in any setting, but allowing a person to access care from the comfort of their home could reduce some of the traditional barriers to connecting with such a team.
While more research is needed to understand the differences between in-person and telehealth treatment of obesity, there is reason to believe that telehealth can be just as beneficial as an in-person appointment. Pre-pandemic studies of telehealth weight management strategies showed high patient satisfaction and engagement. Research consistently shows that more frequent care team interactions lead to more weight-loss. Because virtual appointments can be more frequent, with no need to take time off from work or arrange childcare, telehealth might enable increased contact and therefore improved results. Weight treatment programs across the country are reporting that telehealth during the pandemic enabled them to deliver great care and great results.
How to Find Obesity Care that Incorporates Telehealth and is Right for You
As telehealth continues to become more popular, it’s important to do your research to decide which program is right for you. Below is a list of questions that you might want to ask your healthcare provider before beginning telehealth:
Who will be providing my medical care?
Will you be evaluated by a doctor who is medically trained to treat obesity and has certifications that show that training? (Ex: American Board of Obesity Medicine Certification) Do they have a license in your state and other reputable credentials? This information should be available, so if it is very difficult to find, that may be a red flag.
What is the care model?
Different programs offer different services. Who will you be working with regularly? How often will you see a doctor? How often do you meet with and communicate with a Registered Dietitian? Is working with a health coach part of the program, and if so, what are their credentials?
What do telehealth appointments look like?
Are appointments via video or phone? Or a check-in by email or questionnaire? Telehealth can mean different things as we reviewed earlier, so what can count legally as a check-in may be different from what you envision. It’s important to use a model that works for you.
What kind of support do I receive?
Does the medical weight-loss program offer one-on-one support, community support or a mixture of both? How do you ask questions of your care team in between appointments?
How long does the support last?
What happens once you meet your weight-loss goals? Is there a maintenance phase to help you focus on keeping the weight off long-term?
What technology does the program use?
Before signing up, ask in advance what kind of technology you need to use for your virtual appointments or check-ins. Does it require a computer or a phone? Is there a mobile app? Pick a program that is easy to incorporate into your life.
Is there an option or a requirement for in-person visits?
Some programs require starting with an in-person visit, and sometimes for follow-ups. Others are fully virtual. There may be pros and cons with each, so be sure you know what will be expected of and available to you.
What is the cost?
Cost structures vary greatly. Be sure you understand all the possible costs and beware of anything that signals there may be additional hidden costs. Are services covered by insurance or self-pay? Can you cancel if you are not satisfied?
The Future of Telehealth
Telehealth represents a tremendous opportunity to expand access to expert care for obesity and could help people achieve a healthier weight to improve their health. As new obesity treatment options emerge, asking the questions outlined in this article can help you find a program that will bring you long-term success. While we will need more research to better understand how telehealth can help the obesity epidemic, the future looks bright!
About the Author:
Florencia Halperin, MD, MMSc, is an endocrinologist who completed her training at Harvard Medical School. She is the Chief Medical Officer at Form Health and former Co-Director of the Center for Weight Management and Metabolic Surgery at Brigham and Women’s Hospital. Dr. Halperin is passionate about helping people lose weight as a way to better their health. She has been selected as a Castle Connolly America’s Top Doctor and Boston Magazine’s Top Doctor for several years, including 2020.
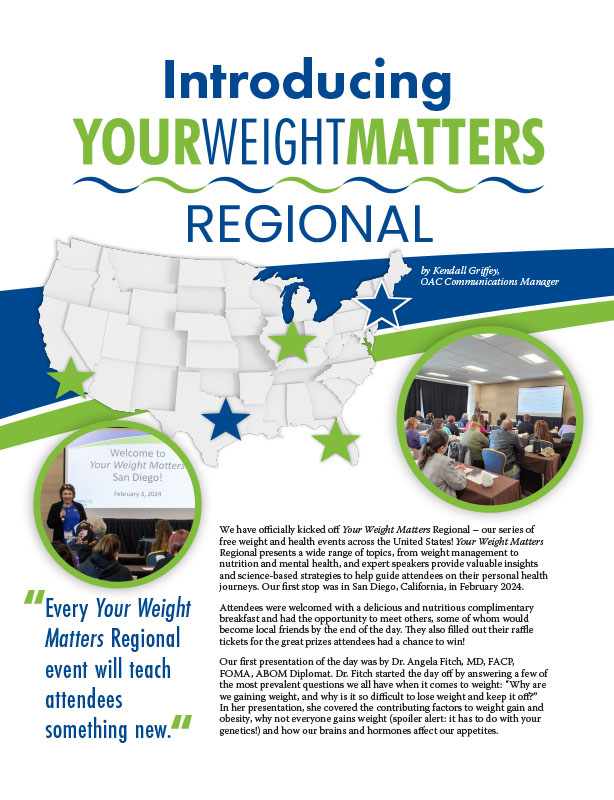
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read Articleby Rachel Goldman, PhD, FTOS; Sarah Muntel, RD; and Stefanie Trilling Winter 2024 This section of Weight…
Read Articleby Maria Paula Guzman, MD Have you ever wondered why shedding a few pounds can be an…
Read Article