Signs, Symptoms and Forms of Postoperative Addiction

by Kelly Broadwater, LPA, LCMHC, CEDS-S
Winter 2023
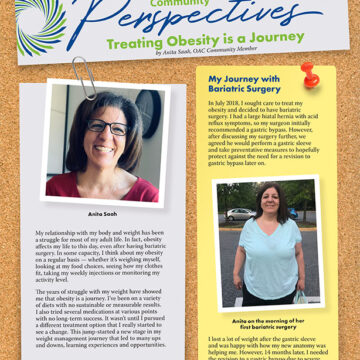
Postoperative addiction has also been called addiction transfer or cross-addiction in the popular press, assuming that individuals “trade” compulsive eating (which becomes restricted after weight-loss surgery) for other compulsive behaviors. However, this fails to fully account for all post-op addiction cases and is seen as an overly simplified way to explain how addictive processes occur after surgery. It is important to note that addictions can develop in patients who did not have any problems before surgery. It is also not uncommon for someone to relapse with prior addictions.
Signs and Symptoms
Addictions that may develop or relapse postoperatively include alcohol, other drugs, and “process” or behavioral addictions such as compulsive spending, sex, gambling, skin picking and overexercise. It is also common to see a relapse of binge eating disorder, with a subset of patients being classified as “food addicts” on the Yale Food Addiction Scale.
The following are some signs and symptoms of addictive behavior:
- A need for more and more of the behavior/substance to achieve the desired effect
- Using the substance or engaging in the behavior for longer than intended, or in higher amounts than desired
- A strong desire to cut back on the behavior/substance, or unsuccessful efforts in changing the drinking/using behavior
- Any social, professional, personal, financial or legal problems related to the addictive behavior
- Other people have commented or complained about the behavior, or others have suggested that the person cut back.
- The person affected is sneaking around, or lying, to cover up the behavior and the consequences of it.
- The person affected is spending more and more time/money to get the substance or engage in the behavior.
- Feelings of guilt or shame about the behavior
- Defensiveness or denial when others confront the person about their behavior
- The behavior or the substance becomes one of the main things the person looks forward to.
There are a variety of free assessments online to screen for various addictions:
- Screening.MHANational.org/screening-tools/addiction/
- CentraHealth.com/sites/default/files/yale-food-addiction-scale.pdf
- Psychology-Tools.com/test/bergen-shopping-addiction-scale
- JenniSchaefer.com/wp-content/uploads/2013/05/Compulsive-Exercise-Test.pdf
- Psychology-Tools.com/test/sast
- Psycom.net/gambling-addiction-test/
*Please note: These tools are only a starting point for identifying problematic and addictive behaviors and are by no means a substitution for professional evaluation and help.
What Can Cause Postoperative Addiction?
There are many psychological and behavioral risk factors for post-op addiction. According to an article about bariatric surgery and lessons learned from COVID-19, periods of high stress or major transition following surgery can make one more vulnerable to using compulsive and addictive behaviors as a way to cope. We saw this in our practice during the COVID-19 pandemic, which has been echoed in preliminary research. Other risk factors include:
- A prior history of addiction
- A family history of substance abuse
- A history of chronic pain and/or the use of narcotics for pain management
- A history of trauma
- Lack of support
- Feelings of isolation, avoidance or self-sabotaging tendencies
- A history of an eating disorder (up to 50% of people who seek treatment for severe obesity have a binge eating disorder)
Alcohol Use Disorder
The most common post-op addiction is alcohol use disorder. Post-op alcohol use prevalence is roughly 10%. What’s more alarming is that research has found that new onset substance users ranged from 34.3-89.5%. Problematic alcohol use tends to increase the further out from surgery you are. It should be noted that studies have shown that both the Roux-en-Y Gastric Bypass and Gastric Sleeve surgeries alter the way alcohol is metabolized postoperatively, which can cause serious medical issues.
Medical complications include:
- Weight regain
- Too much weight-loss
- Dehydration
- Vitamin deficiencies (especially thiamine)
- Ulcers
- Elevated liver enzymes
- Pancreatitis
- Chronic constipation (narcotics especially interfere with the GI tract)
- Hypoglycemia
- Poor sleep
- Mood changes
- High blood pressure
- Negative interactions with medications
- Death
Alcohol withdrawal can be deadly, so it is extremely important that someone who is detoxing has appropriate medical supervision. Anyone dealing with post-op alcohol abuse is advised to seek professional help. Follow up with your surgeon, dietitian and therapist and consider becoming involved in support groups.
Food Addiction
Food addiction is considered a somewhat controversial topic because it is not an actual diagnosis or a formal eating disorder. Food addiction could likely be more accurately called “eating addiction.”
The triad of addiction indicates that people experience a loss of control while using a substance when it no longer provides enjoyment, such as eating to the point of feeling sick or having stomach issues. They also “use” despite negative consequences such as feelings of guilt, shame, and/or medical problems. Lastly, they find themselves preoccupied with the drug of choice or addictive behavior they are involved in, such as someone actively planning their next meal or binge.
Behaviors such as these seem to occur in a subset of patients with binge eating disorder who act in ways that are very biologically driven. These patients demonstrate high levels of impulsivity and compulsivity and are often resistant to intervention, potentially requiring medication to manage their symptoms. They may score high on the Food Addiction Scale and describe their eating as “out of control” and identify with feeling “obsessed” with food and eating. If you fall into this category, you have a higher risk of struggling with weight issues and are more likely to be diagnosed with depression, Attention Deficit Disorder (ADD) or Post-Traumatic Stress Disorder (PTSD).
Health care providers who specialize in binge eating can help you with recovery. Visit AllianceforEatingDisorders.com/find-treatment to learn more and search for help.
Behavioral Addictive Disorders
The research on behavioral addictive disorders such as shopping, gambling, skin picking and so forth is very limited. A 2015 study titled “Addictive Disorders after Roux-en-Y Gastric Bypass” showed that 9.5% had a diagnosable post-op disorder — 31.6% of whom had no previous history.
Unfortunately, follow-up research has yet to be conducted on larger samples to effectively understand more about the risk for non-substance-related addictive disorders. However, even with minimal information and research out there, we know these addictive issues exist in post-op patients. If you struggle with them, you are not alone. The key is finding appropriate professional help for the specific addiction you are dealing with. It’s also important to be assessed and treated for any underlying conditions that could be contributing to your addictive drive.
What Should You Do if You Think You Have a Problem?
The first step requires bravery: admitting what you are struggling with. Talk to someone you trust to break the secrecy of your problem and increase your support. Tell your doctor and other health care professionals so they can help ensure your safety and well-being. Seek professional counseling with an addiction specialist or a therapist familiar with bariatrics.
It can also be instrumental to gain support from others who have experienced similar journeys. Look into what your community offers in terms of 12-step programs such as Alcoholics Anonymous (AA), Narcotics Anonymous (NA), Gamblers Anonymous (GA), SMART Recovery or faith-based Celebrate Recovery. Since the COVID-19 pandemic, many more meetings are accessible online.
Here are some resources for getting started:
- ObesityAction.org
- ObesityHelp.org
- TheRecoveryVillage.com
- Samhsa.gov/find-help/national-helpline
- AA.org
- SmartRecover.org/community
- CelebrateRecovery.com
Please know that you are not alone, help is out there, and there is hope for recovery! Recovery isn’t easy, but it’s worth it. You are worth it!
About the Author:
Kelly Broadwater, LPA, LCMHC, CEDS-S, is a psychologist and certified eating disorder specialist who has treated post-operative bariatric surgery patients for nearly 20 years. She is passionate about providing effective bariatric aftercare and does so at her practice, The Chrysalis Center for Counseling & Eating Disorder Treatment. Kelly frequently presents on topics related to post-op addiction and eating disorders. She enjoys educating other healthcare professionals and is currently co-authoring a book to be published in 2023.
by Robyn Pashby, PhD Winter 2024 “No one is ever going to date you if you don’t…
Read Articleby Rachel Goldman, PhD, FTOS; Sarah Muntel, RD; and Stefanie Trilling Winter 2024 This section of Weight…
Read Articleby Ted Kyle, RPh, MBA; and Gwyn Cready, MBA Fall 2023 In a workshop last November, the…
Read Article