Robotic Surgery: Welcome to the Future!

by Walter Medlin, MD, FACS, ASMBS; and Michelle Everly, PA-C, ASMBS
Fall 2021
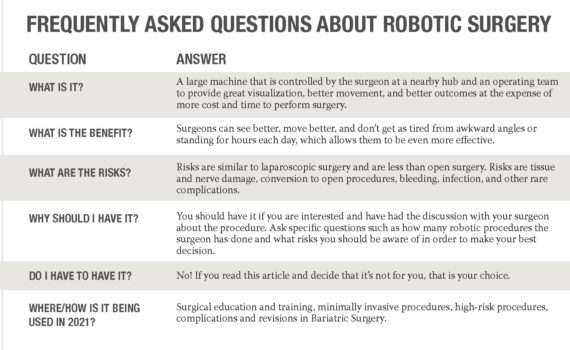
Rosie from The Jetsons and Data from Star Trek are just some of the robots we know and love. They all act in some type of self-guided way. Even the robots that weld your car together will perform a series of steps without any input from a human. Surgical “robots” do NOT do that. They really are not true robots at all and are better described as electronically-controlled instruments.
A Patient’s Needs
Based on popular opinions, when having surgery, most patients want:
- Guaranteed safety
- 100% effectiveness
- No pain at all
- No scars at all
Perfect would be nice, but any step closer is pretty cool. Almost every “advance” in surgery makes progress in one of these areas – but sometimes at the cost of some other area. The safest or most effective care may require a lot of travel and be expensive. The most effective care may NOT be as safe. The least scarring may not be as safe or effective. Science is always trying to give the patient the best options and with no compromises, but that doesn’t always happen.
How Was Robotic Surgery Created?
The Defense Advanced Research Projects Agency (DARPA) is dedicated to making HUGE leaps in what can be done with science and technology. They started the work that led to the internet, self-driving cars and space lasers. One of their biggest projects was bringing medical care to the injured soldier in the field. One great way to do this is to have a machine that a surgeon can use from far away but still be virtually right at the patient’s side.
Out of this remote operating room came the “surgical robot.” It doesn’t yet do anything on its own, but it is essentially the computer between the surgeon and the patient. This opens up many exciting possibilities, but only a few have been achieved so far.
What began in the mid 1980’s with robotic joint procedures has expanded to:
- Urology
- OB/GYN
- Oncology
- Neurology
- Ophthalmology
- Cardiothoracic
- Pediatrics
- General surgery
- Bariatrics
Many commonly performed procedures are ventral hernia repairs, prostate removals, tumor removals and weight-loss/bariatric operations of all types (especially complex revisions).
The cost of doing research and expanding options takes lots of time and effort, and safety has to be proven at every step. Over time, many operations in many specialties have been acceptable for “risk/benefit,” but there is constant debate – as there should be. Technical advances that don’t help a patient are somewhat pointless – like a surgeon in New York taking out a patient’s gallbladder in France – but they can make us think differently, and that may lead to other unexpected benefits.
The Technical Aspect
A robot is not an independent thinking machine that performs surgery at the press of a button, like a microwave. Instead, the robot is an accessory that allows better visualization of tissue and the ability for the surgeon to have near-complete control. Movement and precision are vastly increased. For visualization, try to only use your thumb and pointer finger to pinch and rotate/twist whatever you pick up for the next hour. Compare that to using your entire hand and wrist with all the intricacies of bending and rotating them as well. That is the biggest difference between laparoscopic and robotic surgeries.
In bariatric surgery, the procedure is started laparoscopically. Robotic arms are connected and the surgeon sits at a hub and controls all aspects of movement, including cautery and suturing within the abdomen. The operating team is right at the patient’s side, assisting with changing instruments and communicating with the surgeon directly via microphones and speakers.
From the surgeon’s standpoint, he/she is able to sit for the duration of the robotic portion with an amazingly high-definition picture that is rendered in 3-D. The mechanics of the robot allow for the surgeon’s movements to be smoothly mimicked by the instruments inside of the abdomen. The robot can use cautery and scissors and allows the surgeon to suture with ease. Put simply, the robot is a great tool for the surgeon. It makes the operation smoother and easier for both the patient and the surgeon while keeping everyone’s safety intact.
The Future is Bright
Constant improvements are being made to robotics and to bariatric surgery. When it comes to laparoscopic surgery and robot-assisted surgery, patient outcomes and overall safety are similar. What is now a highly efficient joining of engineering and surgical expertise may one day become the ability to have surgery from a distance. Imagine not having to travel beyond your local hospital while being operated on by an expert robotic surgeon on the other side of the country! In the meantime, have that discussion with your bariatric medical provider about your options to make the best and most informed decision for yourself or for your loved one.
Pros
-
- Better visual view for the surgeon
- Improved efficiency in the work environment and precision/accuracy
- Improved technique with the elimination of a hand tremor
- Surgeons get less fatigued through the procedure and are more capable of performing surgery
- More control for the surgeon
- Equal safety outcomes compared to laparoscopic surgery
- Options for telesurgery
- Less reported pain at incision sites
Cons
-
- More expensive for the hospital (although finance options exist)
- Surgeons go through years of training
- Surgeons can normally feel when something isn’t right, but robots can’t
- Large piece of equipment
- Longer duration of surgery
A Personal Note from Dr. Medlin:
Dr. Medlin has completed more than 500 robotic procedures in the past nine years. He has had two bariatric operations himself in the past two years and neither was with a robot. The choice of WHO performed the surgery was more important to him than the newest technology, even though he sees the merit and usefulness with the robot. Our team has two good friends that are hospital robotic team members. They also had “regular” laparoscopy (we all recovered well!).
None of us would have objected to the robot. Still, none of us would have forced an expert laparoscopic surgeon to work with an unfamiliar tool. Do not feel like this is a tool you are missing out on, but instead, keep an open mind to all options and keep an eye out for how bariatric surgery will change in the next decade to make it better for YOU!
About the Authors
Walter Medlin, MD, ASMBS, is a bariatric surgeon in Salt Lake City, Utah and Lehi, Utah. He performs mostly gastrectomy operations, SADI/loop duodenal switch operations and revision surgeries at Bariatric Medicine Institute. He is a grateful member of the Obesity Action Coalition (OAC) and supports his patients with the OAC Chairman’s Council program sponsored memberships. He had sleeve gastrectomy in 2008 and upgraded to SADI in 2019. He had a revision of this in late 2020 and is doing well! Dr. Medlin LOVES to play outside, especially paragliding and kitesurfing. You can find his YouTube channel at “BMIUtah” and “Walter Medlin.”
Michelle Everly, PA-C, ASMBS, has a passion for health and fitness that started early in her life. She obtained her first degree in Exercise Science and used that pathway to become a Master Fitness Trainer in the Army prior to becoming Dr. Medlin’s Physician Assistant. She continues to help promote health and happiness in her patients, adopting a well-rounded approach to tackling obesity using mindfulness, exercise, dietary changes, encouraging sleep hygiene, and working with patients individually to guide them on their path to success.
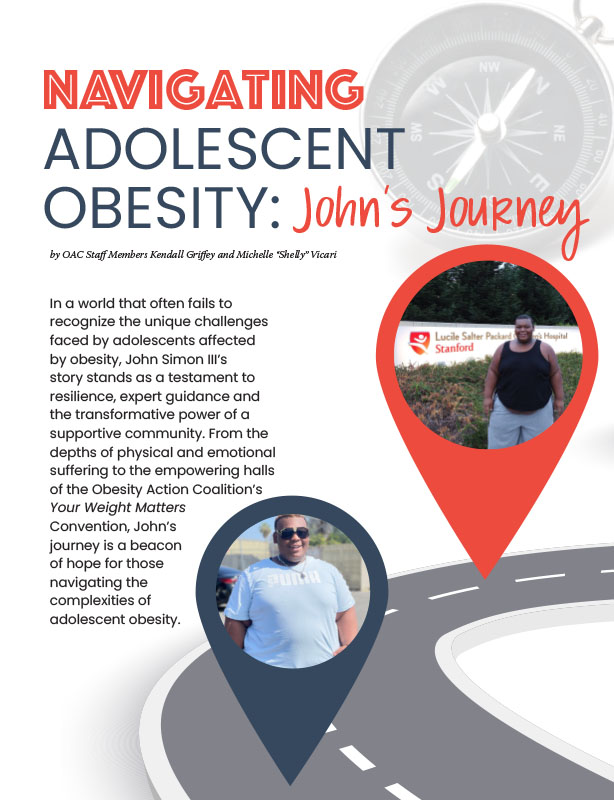
by OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read ArticlePost-operative addiction is often overly simplified as transfer addiction or cross-addiction, assuming individuals “trade” compulsive eating for…
View Video