Reward System and the Brain: To Eat or Not to Eat?

by Sunil Daniel, MD, FTOS
Winter 2017
“There is no sincerer love than the love of food.” – George Bernard Shaw
We need food for energy to keep us alive. Our body and brain are highly efficient in managing the complex process of getting energy from the food we eat (intake) and in using it for sustaining life (output). This process, known as energy balance, is controlled by our brain and keeps our body weight within a certain range.
However, energy balance is also influenced by other factors such as environment, genetics, habit, diseases, gut bacteria, medications, and eating for reward or pleasure. When we eat more than what we need, the extra energy is stored in the form of adipose tissue (body-fat). Throughout time, the consumption of excess calories (overeating) can lead to weight gain and obesity.
During 2011 – 2014, 36.5 percent of U.S. adults and 17 percent of U.S. children had obesity. Obesity is now widely seen as a disease and its complications include heart disease, diabetes, cancer, sleep apnea, arthritis and depression, among others. The World Health Organization (WHO) has found it to be the fifth leading cause of death globally.
To Eat or Not to Eat – How Does Our Brain Decide?
Our body weight, energy balance and our drive to eat form a complex, back and forth communicative relationship between our brain, gastrointestinal tract (GI tract), and other organs including fat cells (adipocytes). These signals are primarily located in areas of the brain known as the hypothalamus and the brainstem.
There are two pathways:
- One that drives hunger
- and the other that drives fullness
Each pathway has hormones and neuropeptides (proteins used by brain cells to communicate) associated with it. So, how do we decide when and how much to eat? Over the long run, our body determines how much energy stores (body fat) we have, and over the short run our brain and stomach communicate to determine food availability, hunger and fullness from meal to meal. When these systems are not working correctly, this can lead to eating more than we need and thus results in weight gain.
Also, when an individual voluntarily loses weight, the brain is constantly receiving signals indicating reduced energy stores (body fat). As a result, it does the only thing it knows – increases our hunger drive to make us eat and gain the weight back. This makes losing weight and keeping it off long-term very challenging.
Furthermore, this process is not taking place in isolation. The hypothalamus communicates with the brain’s reward pathway that provides us with the “hedonic” (meaning pleasure-seeking) or rewarding aspects of food. The hypothalamus and reward centers also interact with the brainstem, which tells us about sensory properties of food such as the sight, smell and taste of it. How do these brain connections lead us to overeat and gain weight?
Eating in Absence of Hunger – Cues and Rewards
We all have our favorite foods. For some, it is a bag of salty and crunchy Cheetos and for others, it is sweet foods like ice cream or chocolate. We are conditioned to consume our preferred foods by cues or triggers such as sight, smell, taste and even memories. When was the last time we enjoyed a steak dinner so much that we ordered it for dessert? We don’t do that. The hypothalamus made us crave the steak because it is a good source of protein, but after that steak meal, it is that chocolate cake or ice cream sundae that is more appealing (even though we may be full).
Although humans have the ability to make conscious decisions and choices, many of our actions escape that control. It is normal to want something that tastes, smells and looks very different from…let’s say a steak, especially sweets, because our brain wants to make sure that we don’t keep eating the same food over and over. If all we ate was steak, we would not get any carbohydrates (sugars) that we also need to survive. When we crave desserts after every meal (or even more than one serving at a time), our healthy energy balance tips to “overweight” because we end up eating more calories than we need.
These cravings are the reason why we find ourselves going back to that piece of dark chocolate when we’re not hungry – even when we fully understand the consequences of overeating. Desserts and tasty snacks can be very hard to control because we are born to love sugar and fats (babies love their mother’s milk because it is sweet and fatty). Our brain also knows that fats have more calories, so we won’t likely starve with yummy foods around.
Eating tasty foods enhances our mood. Foods containing sugar and fat makes us feel good because of the Brain Reward System and a neurochemical called dopamine. The signals in this system travel through various areas of the brain. Additionally, other areas in the brain provide us with memories and emotional attachment to tasty foods.
Dopamine also plays an important role in all of these processes. For example, patients with Parkinson’s disease – who have low levels of dopamine in their brain – tend to eat less food. When these patients are treated with drugs that increase dopamine levels, compulsive overeating is seen. Another system that regulates eating of tasty foods is called the μ-opioid (pronounced mu- opioid) system. In studies, stimulating μ-opioid receptors leads to overeating while blocking μ-opioid receptors leads to decreased food intake.
Obesity and Reward System – A Double Edged Sword
It makes sense that increased responsiveness of brain reward systems to palatable food would result in overeating and obesity. Studies show that when exposed to palatable foods like chocolate cake and pizza, individuals with high levels of “reward sensitivity” have more activity in brain regions responsible for food reward.
Individuals with obesity demonstrate similar activation when exposed to tasty food-related cues (like McDonald’s arches) as compared to leaner individuals. It appears that those who are hypersensitive to food- related rewards may be predisposed to overeating and obesity. It is also proposed that throughout time, reward sensitivity decreases and again leads one to overeat to make up for the missing reward. The pleasurable feeling that we experience from eating tasty food decreases over time – resulting in eating a larger volume of tasty food to experience the same pleasurable feeling. Wonder why we often get cravings but not satisfaction afterwards?
Treatment and Future Direction
Lifestyle intervention, which includes diet, physical activity and behavior therapy, is the foundation of obesity treatment. Currently, patients with overweight or obesity can be treated with lifestyle interventions alone or with such interventions in combination with weight-loss medications or bariatric surgery. Lifestyle interventions are successful at delivering medically significant (5–10 percent) weight-loss, but maintaining this weight-loss is challenging throughout the longer term.
Following weight-loss, there are compensatory changes in the energy balance system that result in increased hunger that favors weight regain. Being constantly hungry in an environment that promotes the constant availability of high-fat and high-sugar foods makes it challenging for people to maintain the weight-loss long-term. The problem is much worse for those who also have problems regulating their sensitivity to food rewards and cues. They must learn to constantly be aware of this high sensitivity and maintain the newly learned behaviors long-term. Medications have been shown to assist individuals in sustaining weight-loss and maintaining lifestyle changes long-term.
Since 2012, there have been five new weight-loss medications approved for the treatment of obesity by the U.S. Food and Drug Administration (FDA). These include:
- Phentermine/Topiramate Extended Release (ER) (Qsymia®)†
- Naltrexone ER/Bupropion ER (Contrave®)†
- Liraglutide (3 milligram) (Saxenda®)†
- Phentermine HCl (8 mg) (Lomaira®)*
* Approved for short term use † Approved for long term use
While the exact mechanism of action for some medications is not fully understood, these medications act on the hunger and fullness pathways while helping to combat adaptations that drive weight gain. For example, the combination Naltrexone ER/Bupropion ER (Contrave®) works in the brain by reducing appetite. Additionally, naltrexone blocks opioid receptors in the brain to decrease the reward aspects of tasty foods.
Much progress has been made recently in identifying brain systems involved in overeating of tasty high-sugar, high-fat foods and weight gain. We are also beginning to understand the genetic differences in food reward systems that predispose certain individuals to diseases like obesity. In recent studies, brain stimulation techniques are also reducing food cravings and eating of tasty foods. Learning more about how the brain, body hormones and genes control different aspects of food intake will lead to better obesity treatments. It can also help change our own mindset (and that of others) that self- control and willpower have anything to do with obesity.
About the Author:
Sunil Daniel, MD, FTOS, is a board certified obesity medicine physician with fellowship training in clinical nutrition and obesity management. He is a fellow of The Obesity Society and has authored several scientific papers on obesity and its medical management. He also serves on the OAC Education Committee.
References:
- Bray, G. & Bouchard, C. Handbook of Obesity-Volume 1: Epidemiology, Etiology, and Pathophysiology. Fourth Edition, 2014. CRC Press.
- Levi J. et al. The State of Obesity: 2014. Better Policies for a Healthier America. Publisher: Trust for America Health.
- Kenny P. J. Neuron 2011; 69:664-679.
- Soleymani T., Daniel S, and Garvey W.T. Maintenance of weight loss. Obes Rev. 2016 Jan;17(1):81-93.
- Burgess, E., Sylvester, M., Morse, K., Amthor, F., Mrug, S., Lokken, K., Osborn, M., Soleymani, T., and Boggiano. Effects of transcranial direct stimulation (tDCS) on binge-eating disorder. M. Int J Eat Disord. 2016; 49: 930-936.
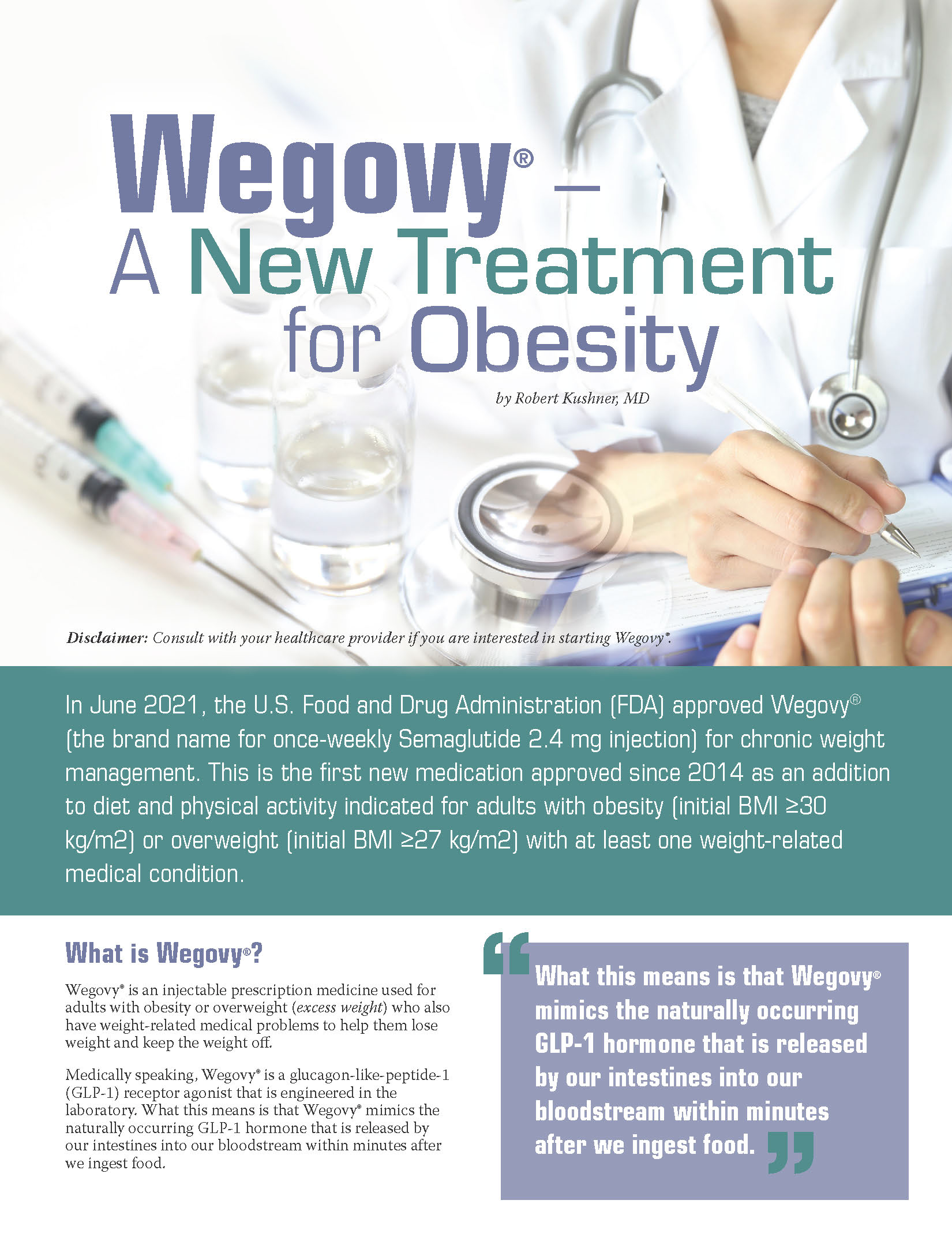
by Robert Kushner, MD Fall 2021 Disclaimer: Consult with your healthcare provider if you are interested in…
Read ArticleFall 2021 While we can’t always control what happens to us, we can choose how we respond.…
Read ArticleThe Obesity Action Coalition (OAC) and the American College of Physicians (ACP) are proud to offer a…
View Guide