Polycystic Ovarian Syndrome (PCOS) and Obesity

by William Hignett, MPH and Ted Kyle, RPh, MBA
Spring 2011
Most individuals are familiar with the common health risks linked to obesity, including type 2 diabetes, sleep apnea, coronary artery disease (CAD), high blood pressure and cancer; however, fewer know that women affected by obesity are also more likely to face reproductive problems like polycystic ovarian syndrome (PCOS).
What is PCOS?
PCOS is one of the most common hormonal disorders in women of reproductive age, affecting 5 to 10 percent. Women with PCOS have irregular menstrual bleeding and often have difficulty getting pregnant. The syndrome occurs when levels of hormones are abnormal. The name “polycystic ovarian syndrome” refers to the appearance of small cysts along the outer edge of the enlarged ovaries of women with this condition.
What Causes PCOS?
The exact cause of PCOS is unknown, but experts believe it is related to the production of an excess amount of androgens, a group of male sex hormones. Although all women produce some androgens, too much of this type of hormone prevents ovulation. Excess androgens also disrupt the normal menstrual cycle. They may cause infertility, acne and abnormal hair growth, such as excess facial hair or male pattern baldness. But, what causes a woman to produce excess androgens?
Many factors may play a role in the production of androgens, and thus the development of PCOS. For instance, excess insulin (the hormone that allows cells to use sugar) may be a factor in developing PCOS. Excess insulin leads to insulin resistance, which in turn decreases your ability to use insulin effectively. When the body cannot use insulin properly, it secretes more insulin to make glucose available to cells. The resulting excess insulin is thought to additionally boost androgen production by the ovaries.
Low-grade inflammation is another potential factor leading to PCOS. Research has shown that women with this condition often have low-grade inflammation. Heredity is also a factor. If your mother or sister has PCOS, you may have a greater chance of having PCOS.
Finally, even conditions before birth in the mother’s womb can be a factor contributing to PCOS. Excessive exposure to male hormones (androgens) in fetal life may permanently prevent normal genes from working normally. These androgens can promote a male pattern of abdominal fat distribution, which increases the risk of insulin resistance and low-grade inflammation. Because many factors can lead to the development of excess androgens, which is related to the development of PCOS, it is impossible to name a single, exact cause of this condition.
Does being Overweight Cause PCOS or Does PCOS Result in Obesity?
Both are possible. The link between PCOS and obesity is complicated. Signs and symptoms of polycystic ovarian syndrome begin for some females soon after they start having periods. Women with PCOS produce too much insulin, or the insulin they produce does not work as it should. The inability of insulin to function normally is one reason why women with PCOS tend to gain weight or have a hard time losing weight. For others, PCOS develops later on, following substantial weight gain. What is clear is that women affected by obesity have a greater risk for PCOS and women with PCOS have a greater risk for obesity.
What are the Symptoms of PCOS?
Although the symptoms vary from individual to individual, a diagnosis is usually made after two of the three following symptoms are found: menstrual irregularity, excess androgen and polycystic ovaries. Since there is no definitive test for PCOS, a doctor diagnoses this condition by ruling out other possible disorders. The physician’s diagnosis is based on findings from your medical history, physical and pelvic exam and pelvic ultrasound. Women diagnosed for PCOS also undergo blood tests that measure levels of several hormones in order to exclude potential causes of menstrual abnormalities or androgen excess.
Addressing Your Overall Health as Part of the Treatment for PCOS
Quitting smoking is generally the most positive action you can take to improve your health, and related to PCOS, it may lower the higher levels of androgens. Birth control pills and androgen reducing therapies can address the symptoms of PCOS, such as menstrual cycle problems, male-type hair loss and hair growth and acne. For women who wish to get pregnant, fertility drug treatment may also help start ovulation. For some women, a doctor might also prescribe the anti-diabetic drug metformin, or the fertility drug gonadotropins, to address insulin resistance.
And importantly, even modest weight-loss of 5 to 7 percent of body weight throughout six months can lower your insulin and androgen levels. Such a reduction, according to Dr. Huang and associates in the 2007 edition of Berek and Novak’s Gynecology, restores ovulation and fertility in more than 75 percent of women with PCOS.
Why is Early Diagnosis and Treatment of PCOS Important?
As with any chronic disease, finding it early helps a lot. That’s because PCOS makes a number of other diseases more likely. These include high blood pressure, type 2 diabetes, sleep apnea, abnormal uterine bleeding, cholesterol abnormalities, metabolic syndrome, heart disease, cancer of the uterus and complicated pregnancies. With early diagnosis and treatment of PCOS, doctors can reduce risk of these long-term complications.
What Treatments Can Help with PCOS?
No simple cure for PCOS exists. Fortunately, it can be controlled, decreasing the risk of long-term complications. Engaging in regular exercise, keeping a healthy diet, losing excess weight, quitting smoking and using medications to control hormones are all important parts of treatment for PCOS.
Daily exercise improves the body’s use of insulin, and many of the symptoms of PCOS may improve with at least 30 minutes of exercise a day. Furthermore, it is important to fuel your body with a healthy diet – one that includes many complex carbohydrates and is low in animal fats. The more fiber in a food, the slower it is digested, which has the advantage of causing your blood sugar levels to rise slower. Examples of high-fiber complex carbohydrates include whole-grain breads and cereals, whole-wheat pasta, brown rice, barley and beans.
Conclusion
PCOS is a common hormonal disorder that affects women of reproductive age. PCOS challenges the quality of life of the women who suffer from it. Yet with proper treatment, PCOS can be managed and symptoms can be relieved. In addition, early diagnosis and treatment of PCOS can help reduce the risk of long-term complications such as type 2 diabetes, heart disease and stroke. For more information on PCOS, visit the Polysystic Ovarian Support Association at www.pcosupport.org.
About the Authors:
Ted Kyle, RPh, MBA, is a pharmacist and health marketing expert. Ted has worked for more than 10 years on programs and products to help people quit smoking and lose weight. Ted is a member of the OAC National Board of Directors.
William Hignett, MPH, is a disease management expert with a master’s degree in public health from the University of Pittsburgh. He has years of experience as a health educator for universities, hospitals, Fortune 100 companies and health insurers. He has seen first-hand how obesity contributes to many chronic diseases and how weight bias stands in the way of effective solutions.
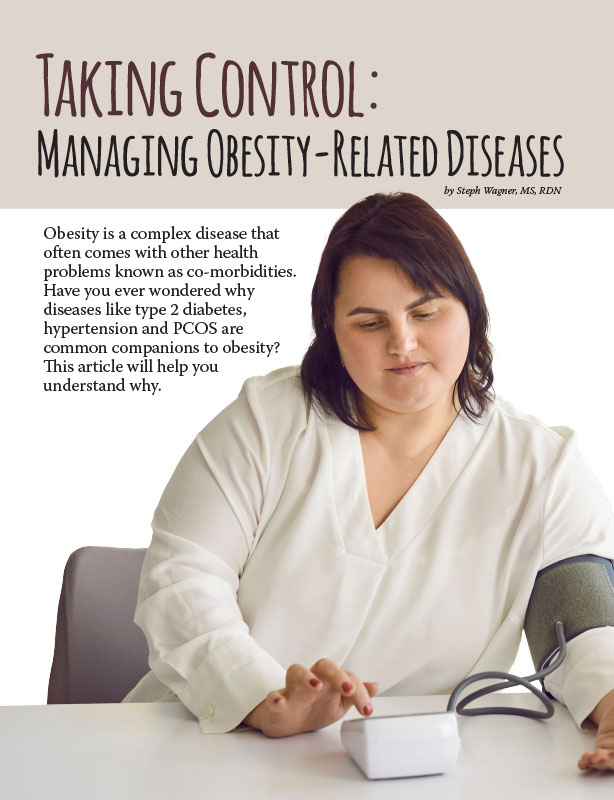
by Steph Wagner, MS, RDN Spring 2024 Obesity is a complex disease that often comes with other…
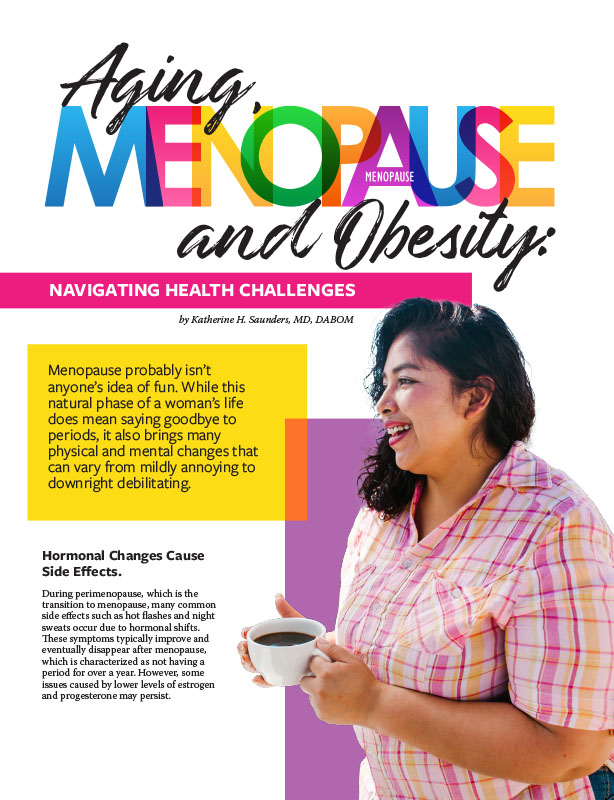
Read Articleby Katherine H. Saunders, MD, DABOM Spring 2024 Menopause probably isn’t anyone’s idea of fun. While this…
Read Articleby Nina Crowley, PhD, RD (with Inspiration from Shawn Cochran) Winter 2024 Dating, no matter your age,…
Read Article