Obesity & Breast Cancer


by Nancy Kushner, MSN, RN, and Robert Kushner, MD
Summer 2013
Obesity and breast cancer are both on the rise worldwide. These two disorders are also linked to one another. Excess body weight, poor diet and physical inactivity have been associated with an increased risk of breast cancer in postmenopausal women. With 70 percent of postmenopausal women in the U.S. estimated to be affected by excess weight or obesity, this is cause for concern.
The good news is that weight management also plays a key role in the prevention of breast cancer and in improving the prognosis once breast cancer is diagnosed. The relationship between obesity and breast cancer, however, is complex and not fully understood.
What do we know about the relationship between excess body fat and breast cancer?
A strong relationship exists between obesity and many cancers, particularly postmenopausal breast cancer. Excess body fat may increase the risk of developing postmenopausal breast cancer through factors that include:
- Insulin resistance
- Changes in the level of sex hormones
- Chronic inflammation
In contrast to postmenopausal breast cancer, the relationship between excess body fat and premenopausal breast cancer is less certain. In fact, some studies showed that excess body fat was protective against developing breast cancer in premenopausal women, though this was not always statistically significant.
We also know that many pre and postmenopausal women, after receiving a breast cancer diagnosis, end up gaining weight. Weight gain and obesity lead to poorer breast cancer prognosis, more obesity-related conditions like heart disease and diabetes and worse surgical outcomes including higher infection rates, poorer healing, lymphedema, fatigue and functional decline.
Why is this important?
Breast cancer is the most common cancer among American women, excluding skin cancer. About 1 in 8 women in the U.S. will develop invasive breast cancer in their lifetime. Understanding the connection between excess weight and breast cancer risk gives individuals more reasons to better manage their weight and decrease risks of developing this all-too-common and life threatening disease. It can also empower individuals to take control of their weight after a breast cancer diagnosis.
Understanding Breast Cancer Risk Factors
A risk factor is anything that increases your risks of developing a disease. Different types of cancer have different risk factors. However, risk factors don’t tell the whole story. Some women can have multiple breast cancer risk factors and never develop the disease, while others may have no risk factors and develop the disease. Still, it’s important to be aware of your breast cancer risk factors and be able to distinguish between the ones you can change, and the ones you cannot change.
Main breast cancer risk factors you cannot change:
-
- Being a woman (breast cancer is 100 times more common in women than in men)
- Aging (two out of three invasive breast cancers occurs in women age 55 and older)
- Genetics (about 5-10 percent of breast cancer is thought to be due to gene defects inherited from a parent)
- Family history of breast cancer (breast cancer risk is higher if a relative has had the disease)
Lifestyle-related breast cancer risk factors you can change:
-
- Alcohol intake (women who consume one drink a day have a slightly higher risk as compared to nondrinkers and women who drink two to five drinks daily have about one and a half times the risk as nondrinkers)
- Being affected by excess weight or obesity (after menopause, this is a significant risk factor)
- Physical inactivity (research is growing in this area to show that physical activity decreases your risk of developing breast cancer)
- Poor diet (diet is modestly associated with breast cancer risk; total calorie intake is positively associated with breast cancer risk; a low-fat and high-fiber diet may be weakly protective against breast cancer)
What can you do to prevent breast cancer?
-
- See your healthcare provider for regular breast exams and breast cancer screening mammograms.
- Control your weight.
- Be physically active by engaging in aerobic activity (a minimum of 150 minutes per week of moderate activity or 75 minutes per week of vigorous activity) and muscle strengthening exercises two days per week.
- Choose a healthful, balanced diet that is rich in vegetables and fruits, lower in saturated fat, higher in fiber and calorie-controlled.
- Limit your alcohol intake.
- Talk to your healthcare provider about your family history of breast cancer and ways to lower your risk.
- Learn about the risks and benefits of hormone replacement therapy.
How can you improve your prognosis after a breast cancer diagnosis?
Survival rates for early-stage breast cancer have improved remarkably with the introduction of new therapies. A woman diagnosed with early-stage breast cancer has a 98 percent chance of being cancer free five years later and survival rates remain more than 77 percent even 10-15 years after treatment.
Weight management is considered a standard of care in women affected by excess weight or obesity diagnosed with early-stage breast cancer. If someone affected by excess weight or obesity is motivated to lose weight during cancer therapy, there is no contraindication to modest weight-loss (of no more than two pounds per week) through exercise and calorie restriction, as long as the oncologist (cancer specialist) approves, weight is closely monitored and no adverse effects are noted. Intentional weight reduction through exercise (aerobics and resistance training) and calorie restriction has been associated with health benefits.
For some cancer survivors, however, intentional weight reduction may be better tolerated once chemotherapy, radiation or surgical therapies are complete. In these situations, preventing weight gain, weight maintenance and preserving, or rebuilding, muscle mass are the recommendations.
Some cancer survivors may unintentionally lose weight as a result of cancer treatment and these patients need to be assessed and managed to improve their nutritional status. Many factors can negatively affect the ability of cancer survivors to engage in exercise, such as severe anemia, severe fatigue or having a compromised immune status which makes going to the gym risky. Under a health professional’s direction, it’s prudent for cancer survivors to avoid inactivity and return to normal activities as soon as possible.
Conclusion
Though the relationship between obesity and breast cancer is complex, we do know that achieving or maintaining a desirable body weight through eating a healthy, well-balanced diet and regular exercise, may be one of the most important lifestyle behaviors in the prevention of breast cancer and to improve survival after a breast cancer diagnosis.
About the Authors:
Nancy Kushner, MSN, RN, is a nurse practitioner, health writer and co-author of Dr. Kushner’s Personality Type Diet and Counseling Overweight Adults: The Lifestyle Patterns Approach and Toolkit.
Robert Kushner, MD, is Clinical Director of the Northwestern Comprehensive Center on Obesity in Chicago, Professor of Medicine, Northwestern University Feinberg School of Medicine, Past President of The Obesity Society, a member of the OAC National Board of Directors, author of more than 180 scientific articles on obesity and nutrition, author of Dr. Kushner’s Personality Type Diet, Counseling Overweight Adults: The Lifestyle Patterns Approach and Toolkit and Fitness Unleashed: A Dog and Owner’s Guide to Losing Weight and Gaining Health Together.
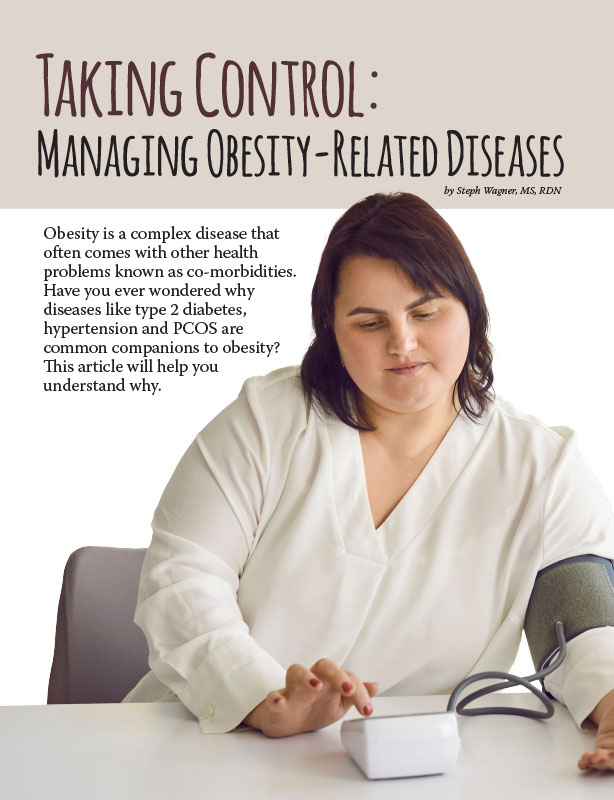
by Steph Wagner, MS, RDN Spring 2024 Obesity is a complex disease that often comes with other…
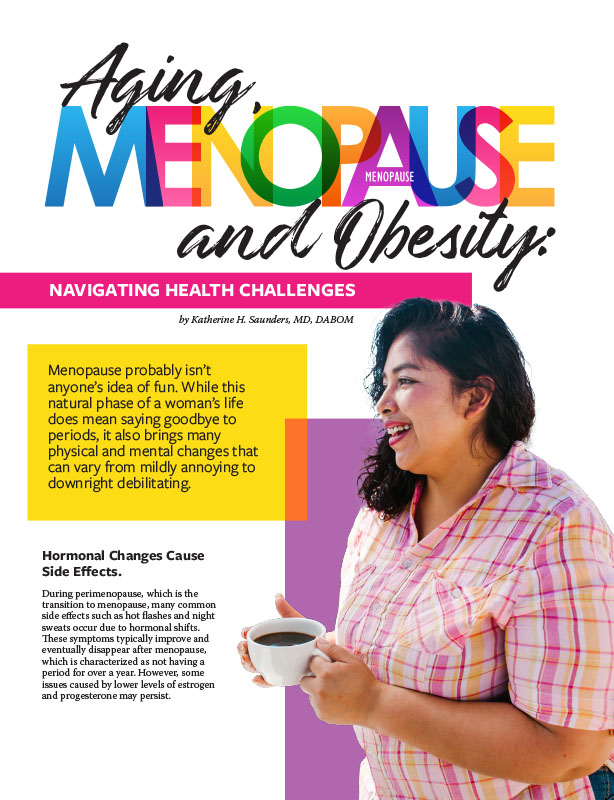
Read Articleby Katherine H. Saunders, MD, DABOM Spring 2024 Menopause probably isn’t anyone’s idea of fun. While this…
Read Articleby Nina Crowley, PhD, RD (with Inspiration from Shawn Cochran) Winter 2024 Dating, no matter your age,…
Read Article