Obesity and Weight Bias in Racial and Ethnic Groups

by Holly F. Lofton, MD; and Shanna Tucker, MD
Winter 2021
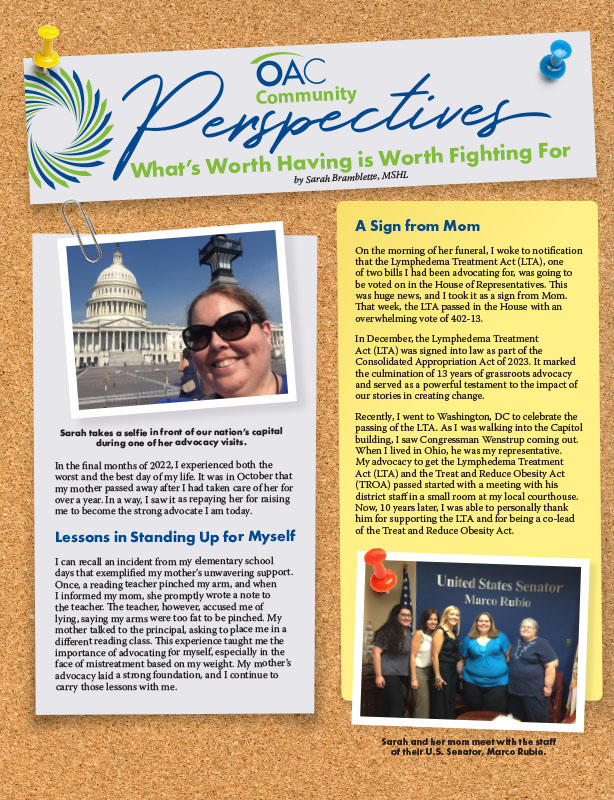
Racial injustice is a public health issue that requires an extensive amount of attention and action. The medical field is of course not immune to such issues. In fact, racial disparities, and other biases such as weight bias, can be found in all areas of healthcare. For example, according to the Centers for Disease Control (CDC), Black Americans continue to experience the highest COVID-19 death rates in the U.S. – two times as high as the rate for Caucasians or Asian Americans.
Additionally, multiple studies done by the Infectious Diseases Society of America have concluded that obesity increases one’s risk for severe infection or even death from COVID-19. It’s time we discuss obesity and weight bias in minority populations.
How Common is Obesity in Racial and Ethnic Groups?
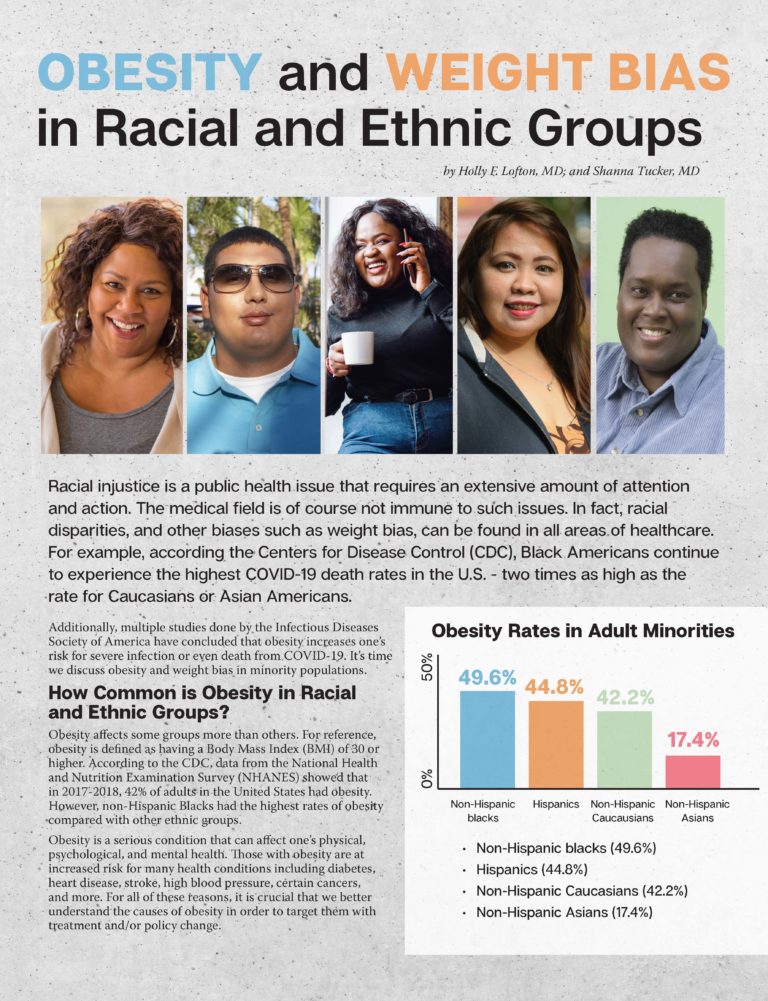
Obesity affects some groups more than others. For reference, obesity is defined as having a Body Mass Index (BMI) of 30 or higher. According to the CDC, data from the National Health and Nutrition Examination Survey (NHANES) showed that in 2017-2018, 42% of adults in the United States had obesity. However, non-Hispanic Blacks had the highest rates of obesity compared with other ethnic groups.
Obesity is a serious condition that can affect one’s physical, psychological, and mental health. Those with obesity are at increased risk for many health conditions including diabetes, heart disease, stroke, high blood pressure, certain cancers, and more. For all of these reasons, it is crucial that we better understand the causes of obesity in order to target them with treatment and/or policy change.
Obesity Rates in Adult Minorities
- Non-Hispanic blacks (49.6%)
- Hispanics (44.8%)
- Non-Hispanic Caucasians (42.2%)
- Non-Hispanic Asians (17.4%)
Why is Obesity More Common in Racial and Ethnic Groups?
There are many factors that can lead to the differences we see in obesity rates among racial and ethnic groups. Some of the main factors include:
- Maternal characteristics
- Genetics
- Nutrition
- Social environment
- Finances
- Education level
- Stressors such as systemic racism
Maternal Characteristics
Maternal health during pregnancy can have a huge impact on a child’s likelihood of developing obesity. Compared to Caucasian women, a greater number of African American and Hispanic women give birth to babies that are overweight or have obesity. Larger babies tend to be born to women with gestational (pregnancy-related) diabetes. Hispanic women have higher rates of gestational diabetes compared to others.
Infants and children with excess weight have a greater likelihood of developing adult obesity. Additionally, young children raised in a household with two parents who have obesity have twice the risk of developing childhood obesity.
Genetics
The role of genes in obesity is commonly studied. There is evidence that some proteins that are common in obesity are more present in African American people than in Africans or Europeans. Therefore, just being born in the United States can play a role in developing obesity. Policy changes to include more African Americans in clinical research for obesity treatments are necessary to determine the best strategies to manage obesity in minorities.
Nutrition
In terms of nutrition, studies have showed that African American and Hispanic children are more likely to be exposed to fast food and sugary beverages before age two. This can be due to several factors. For instance, those of low income and social status are more likely to be exposed to poorer quality diets that contain calorie-dense foods and unhealthy fats.
Families in these communities may also have difficulty accessing fresh, affordable fruits and vegetables due to lack of proximity to their homes or the high costs of such foods. Those of lower economic status may not be able to access recreational sports and are therefore less active. Policy strategies to intentionally bring low-cost healthy foods to disadvantaged neighborhoods have shown promise. More resources for community centers that provide access to physical activity in these communities can help.
Social Environment
One’s social environment can cause internal stress that can lead to inflammatory responses, which can increase the risk for diseases such as obesity. Stress due to lack of income, racism, and poor sleep can cause hormonal changes that are related to obesity.
Finances and Education
Studies have shown that obesity rates can be affected by financial status. However, the relationship between obesity and income or education level is much more complex and differs by sex and race.
The CDC’s Morbidity and Mortality Weekly Report showed that in 2011-2014, rates of obesity were lower among men and women with college degrees. When looking at men and the association between income and obesity, obesity prevalence was lower in the lowest and highest income groups compared with the middle-income group. However, for non-Hispanic black men, obesity prevalence was higher in the highest income group.
In this same report, among women, obesity prevalence was lower in the highest income group than in the middle and lowest income groups.
Weight Bias in Minorities
Weight bias can present itself in many different ways. Sometimes, race and ethnicity can play a key role in how much weight bias you experience and how you view weight bias.
The Obesity Action Coalition (OAC) conducted research in August 2020 on people from minority populations that included Black/African American, Latino/Hispanic and Asian/Pacific Islander communities. They surveyed 517 U.S. Black/African American adults, 530 U.S. Latino/Hispanic adults and 429 Asian/Pacific Islander adults. They found that each group differs in how they handle and view weight bias. Here are some of the things that they found:
- The Latino/Hispanic respondents were more likely to report that weight stigma has an effect on their ability to maintain/control their weight.
- The Black/African American respondents agreed less with blaming people with obesity for their weight than did the Asian/Pacific Islander group.
- Asian/Pacific Islander respondents were less likely than other groups to say they hold no stereotypes about people with obesity.
- More Black/African American respondents than Asian/Pacific Islander respondents thought that race and ethnicity plays a role in how healthcare providers treat people with obesity.
Through this research study, the OAC found that Black/African American people may experience more weight bias from their healthcare providers, which can negatively affect their care. Weight bias is extremely harmful to a person’s mental, social, and physical health, and unfortunately, it has been shown that one’s race and ethnicity could determine how often one experiences weight bias and where one experiences it.
Putting it All Together
In conclusion, there are many reasons why rates of obesity and weight bias are different in racial and ethnic groups. These differences range from factors present even before one has left the mother’s womb to environmental factors and food choices.
The authors of this article encourage readers to be aware of the similarities between weight bias and ethnic and racial bias. One way to start addressing these disparities is by treating obesity appropriately, which will also help prevent and/or treat health conditions related to obesity. For readers who have obesity, the very first step to treating obesity is talking about it. If your doctor has not brought it up, we encourage you to ask your doctor about your weight at your next visit or ask to schedule a visit dedicated to discussing your weight and how it may be affecting health. You can also use the OAC’s Your Weight Matters toolkit to initiate the conversation about weight with your healthcare provider and to determine if there is a treatment option or approach that works for you.
About the Authors:
Holly F. Lofton, MD, is a Clinical Associate Professor of Medicine and Surgery at NYU Langone Health where she has served as Director of the Medical Weight Management Program at NYU Langone Health since 2012. In 2016, she became a founding member of the NYU comprehensive program on obesity and leads the education and clinical access divisions of the program. She is also the Program Director of NYU Langone Health’s Clinical Obesity Medicine Fellowship.
Shanna Tucker, MD, grew up in Los Angeles, CA and completed her undergraduate degree at the University of California-Berkeley. She obtained her medical degree from Harvard Medical School and completed an internal medicine residency at Weill Cornell Medicine with a focus in primary care. Currently, she is the Obesity Medicine Fellow at University-Langone.
by Robyn Pashby, PhD Summer 2023 To do something a little different, I’d like to begin this…
Read Articleby Elizabeth (Liz) Paul Summer 2023 I have lived with obesity my entire life. Reconciling the size of…
Read Articleby Sarah Bramblette, MSHL Summer 2023 In the final months of 2022, I experienced both the worst…
Read Article