Obesity and the Immune System

by Stephanie F. Deivert, RD, LDN, and Mildred K. Fleetwood, PhD
Winter 2013
It is now general knowledge that obesity has an effect on various other diseases including diabetes, cardiovascular disease, high blood pressure, high cholesterol, cancer, sleep apnea and more recently, fatty liver disease; however, did you ever think that obesity could affect your immune system?
Recent studies in humans and animal models affected by obesity have shown an impaired immune response or immune function leading to increased chances for various infections. The cause of this has not been well defined. Let us review what is currently known about this possible harmful effect that obesity has on the body.
Nutrition and Immune Function
We have all heard, “Eat an apple a day; you will keep the doctor away.” This is actually true. Studies do show that eating a diet that is high in fiber and antioxidants (fruits and vegetables) and has enough protein helps to keep your immune system working properly. Specific micronutrients such as iron, selenium, zinc, copper, as well as vitamins C, A, E, B-6 and folic acid have important roles in the body’s immune response.
Diets high in sugar and fat, or eating too many calories in general, make you more prone to infection. This is because it can lead to increases in blood sugar or may cause oxidative damage. Oxidative damage is an overproduction of reactive oxygen species compared to the body’s ability to detoxify cells. This type of damage from oxygen increases your chances of infection.
If you have too little protein intake, you are also at risk for protein-energy malnutrition. This has also been associated with significant impairments of immunity. It is commonly thought that deficiencies or malnutrition cannot happen in an individual affected by obesity; however, deficiencies and malnutrition happen because of a poor diet. Therefore, deficiencies could very well occur in any individual who eats poorly, no matter their weight.
So what can you do with your diet to help your immunity?
- If you are affected by obesity, decrease your calories to help facilitate weight-loss.
- Decrease simple carbohydrates such as sweets, goodies, baked goods, sugar-sweetened beverages, sugar, honey, jams, jelly, etc.
- Decrease excess “bad” (saturated or trans) fats commonly found in: commercial baked goods, processed or fried foods, cheese, whole and 2% milk, ice cream, cream, fatty meats (beef and pork products), butter and margarine. Bad fats are also found in some vegetable oils – coconut, palm and palm kernel oil.
- Eat two cups of whole fruit per day and at least three cups of vegetables per day.
- Drink or eat three cups of low-fat (1% or skim) liquid dairy or dairy alternative per day (light yogurt, low-fat or fat-free milk). Eat two to three ounces of lean meat or beans with two meals per day (three ounces = deck of cards).
- Drink at least 60 to 80 ounces of water per day.
Exercise and Immune Function
Exercise and health go hand-in-hand. We have all heard that exercise helps fight diseases such as high blood pressure and cholesterol, cancer, sleep disturbances, mood and obesity itself. In general, people who exercise and are physically active throughout the day tend to live longer, healthier lives. There is also evidence that exercise does improve immune function. Studies have shown that exercise seemed to increase numbers of certain immune cells that help to bolster immune activity.
Moderate exercise has been reported to increase certain immune cells, reducing the risk of infection. On the other hand, too intense of exercise (without adequate rest) has actually been shown to increase stress on the body and cause a person to be more at risk to infection.
For a great list of resource articles on exercise, please visit the “Past Articles” section located in the “Your Weight Matters Magazine” section on the OAC Web site at www.obesityaction.org.
Obesity and Immune Function
A person affected by obesity that eats healthy and exercises is still at risk for decreasing immune function. Obesity itself has been shown to impair immunity in some studies. Some of these specific findings include:
- Decreased cytokine production
- Altered monocyte and lymphocyte function
- Natural killer cell dysfunction
- Reduced macrophage and dendritic cell function
- Decreased response to antigen/mitogen stimulation
Now, you may be saying to yourself, “What does all that mean?” The bottom line is studies have shown impaired immune response in animals and people affected by obesity, leading to increased risks of infection. The exact cause of these findings is not known. Obesity is an extremely complex disease and many processes and pathways are altered, any of which could affect the immune system.
Population studies have shown the same things. For instance, hospitalized patients affected by obesity are more likely to develop secondary infections and complications, such as sepsis, pneumonia, bacteremia, and wound and catheter infections. Overall, it appears that obesity may increase the risk for bacterial and viral infections. Severe obesity, in and of itself, has also been named a risk factor for increased severity of infection and death from the H1N1 influenza strain. Those affected by obesity may also be at risk for viruses like H1N1 because of less of an immune response to vaccinations, although it has not been studied to date.
Vaccines and Obesity
Some studies have described relationships between vaccine response and obesity. Vaccines work by introducing a killed or weakened form of the disease to the immune system. The killed or weakened disease is not strong enough to produce symptoms or signs of the disease, but the vaccine does stimulate production of antibodies to protect against the disease if you come in contact with it in the future.
A lot of work has been done regarding hepatitis B vaccines in regards to obesity, in which studies show strong evidence that individuals affected by obesity have a very high non-response rate to vaccination. This means after the introduction of the “non-active virus” to the individual’s immune systems, the disease-fighting antibodies are not produced to the extent they need to be to protect against the disease.
In a person affected by obesity (body mass index [BMI] of 30-39), studies have shown that it takes a more potent hepatitis B vaccine in order to come close to the response rate of a standard single-dose therapy in an individual with a BMI less than 30 (overweight).
Conclusions
The exact cause of how obesity affects the immune system is unknown. One theory is the type of fat that you have, as not all fat is created equal. White adipose tissue (WAT) is usually found in higher levels in people who are affected by obesity. Several studies show that WAT has many functions, including regulation of inflammatory processes. When the body has excess WAT, chronic inflammation makes it harder for the body to fight off infections.
Well known links exist between diet, exercise and immune function. Eating healthier and incorporating moderate exercise can help to increase your immune function; however, now it is known that obesity itself (diet or genetic induced) decreases immunity leading to increased risk of bacterial and viral infection as well as decreased responsiveness to some vaccinations. The exact mechanisms are not known; however, future studies will focus on this area. The good news is that several studies have shown an increase in immune responsiveness and improvements after weight-loss or following dietary restriction.
About the Authors:
Stephanie F. Deivert, RD, LDN, has been with the Center for Nutrition and Weight Management at Geisinger Health System since 2002. She completed her bachelor’s in Nutritional Sciences and Exercise Physiology at Penn State University in 2002 and her dietetic internship at Geisinger Medical Center in 2004.
Mildred K Fleetwood, PhD, (D) ABMLI is one of five board-certified medical laboratory immunologists in Pennsylvania and currently works as a consultant. She directed the immunology based laboratories for the Geisinger Health System for 32 years and taught immunology at the Commonwealth Medical School until she retired in 2011.
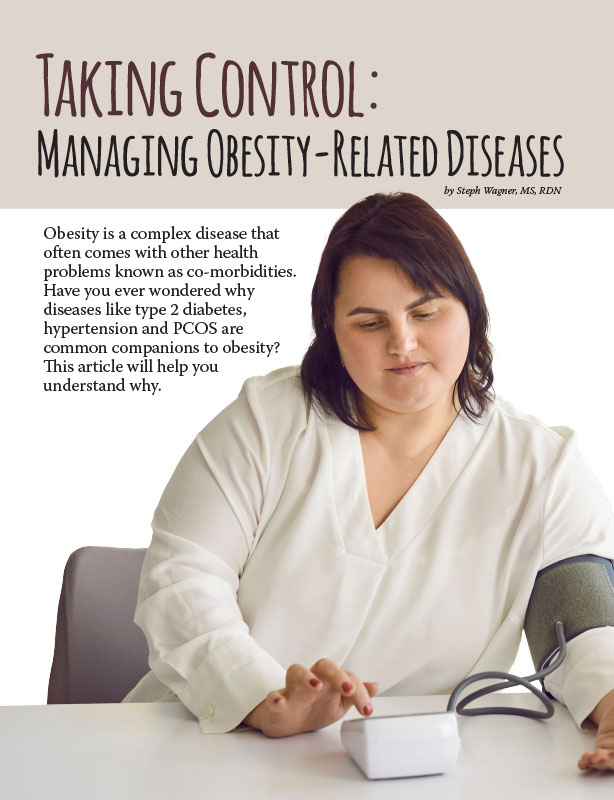
by Steph Wagner, MS, RDN Spring 2024 Obesity is a complex disease that often comes with other…
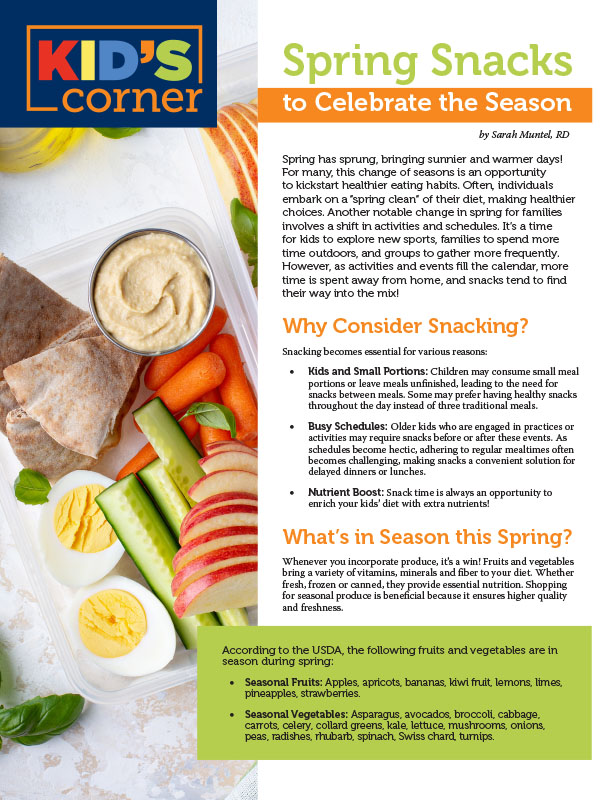
Read Articleby Sarah Muntel, RD Spring 2024 Spring has sprung, bringing sunnier and warmer days! For many, this…
Read Articleby Yelena Kibasova Spring 2024 The fitness world is evolving, with new trends and innovations that promise…
Read Article