Managing Obesity as a Chronic Disease

by Nadia B. Pietrzykowska, MD, FACP
Spring 2018
What Makes Obesity a Disease?
Obesity was officially classified as a disease by the American Medical Association (AMA) in 2013. By defining it as a serious medical condition, the hope was that it would be recognized, diagnosed and treated as such.
Obesity is defined as excess adipose tissue (fat tissue). Fat tissue is a collection of fat cells that have multiple functions, including producing hormones and substances that cause inflammation. This may lead to many disease states like diabetes, fatty liver disease, high blood pressure, high cholesterol, sleep apnea, heart disease and some cancers. When left untreated, obesity can result in disability, decreased quality of life and a shorter lifespan.
What Makes Obesity a “Chronic” Disease?
Abnormalities observed in obesity are complex and involve biological, behavioral, genetic and environmental factors. Some of them may be reversible but others are not, which makes obesity a chronic disease state.
Individuals affected by obesity, as well as healthcare providers specializing in obesity management, know that excess weight is a medical condition that can be controlled but is difficult to “cure.” When successfully losing weight, whether through lifestyle changes, medical management or a surgical procedure, challenges may arise. The biggest of all is successfully maintaining weight that was lost.
During and after weight-loss, many regulatory processes are triggered that can sabotage weight-loss and induce weight regain. Knowledge regarding these mechanisms is growing, but much has yet to be learned. By acknowledging these challenges, both patients and healthcare providers set the path for a more successful weight-loss journey.
In my practice, I notice that if patients understand obesity is a chronic medical condition, they find a sense of relief. They stop blaming themselves. As they accept it, they feel empowered and engage in solutions and treatment options.
How Should this Chronic Disease Be Treated?
As this is a complex condition, there is no “one size fits all” treatment solution. In addition, as challenges may evolve throughout time, treatment solutions should adapt as well. The currently accepted treatment options for obesity are lifestyle modification (nutrition, behavior modification and exercise), weight-loss medications, gastric devices and bariatric surgery.
Here are some of the ongoing challenges that can be faced throughout time:
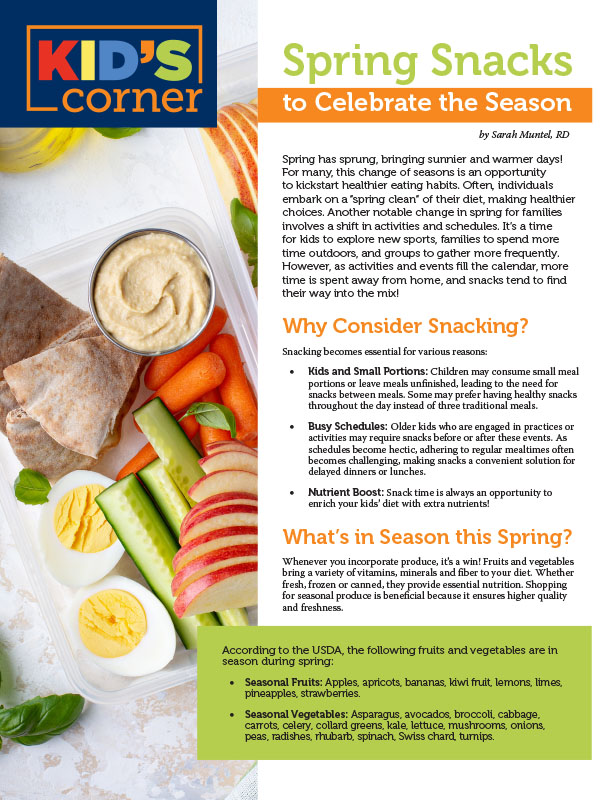
Evolving Nutritional Needs: As individuals affected by obesity lose weight, their nutritional needs change. Caloric goals and food composition (Percent of protein, fats and carbohydrates) need to reflect the body’s needs at different stages of the weight-loss journey.
Building a “good relationship” with food benefits both the body and mind. Unlike with smoking tobacco or drinking alcohol, one cannot “quit” eating. It’s important to keep food interesting, pleasurable and healthy. This way, food consumption will ultimately become a lifestyle and not a “diet.” This will help control weight in the longer term.
Patients that undergo bariatric surgery have very specific nutritional needs as well. Long-term established medical care is important for success in preventing complications and addressing challenges.
Behavioral Challenges: Biological processes that occur during weight-loss are connected with behavioral responses. Food may be perceived as a reward and can sometimes be used to compensate for an emotional void or to cover-up trauma. In these instances, changes in eating can cause significant distress and hinder weight-loss efforts. In addition, decreasing calories or changing the composition of food can trigger uncontrollable feelings of hunger and/or cravings. This results from changing levels of various hunger and satiety hormones.
Sometimes, patients report that they feel ashamed because they can’t stop eating. Little do they know that this hunger is well beyond their control because it is triggered by very powerful biological processes.
Effects on Energy Metabolism: Virtually all processes involved in weight-loss can affect energy metabolism, including:
- Amount of calories consumed
- Food composition
- Length of time someone has been attempting weight-loss
- Aggressiveness of the weight-loss plan
- Individual and genetic variability
These processes are still poorly understood and are also extremely variable from one person to the next. Monitoring the body’s response to weight-loss throughout time is very important. This may cause changes in physical activity and exercise to compensate for variations in energy metabolism.
Obesity Pharmacotherapy: Adaptive mechanisms that occur during weight-loss have been identified and studied. This has allowed for the creation of obesity medications that target specific and common problems such as hunger and cravings. Throughout time, responses to these medications may change. A vigilant healthcare provider treating obesity will adjust or change medications to continue to target problems and help patients achieve their goals. This is chronic management of a chronic disease.
The Benefits and Implications of Bariatric Surgery: In instances where bariatric surgery is the best treatment option, it’s important to understand that it does not “cure” obesity. To avoid weight regain, lifelong obesity treatment is still warranted. Lifestyle changes have to become permanent to ensure success.
In some cases, obesity medications may also be needed to overcome the adaptive mechanisms of the human body. Managing obesity as a chronic disease is crucial for the lifelong success of affected individuals. Using available treatment tools can result in successful “remission” of this
chronic disease.
What Are the Barriers to Managing Obesity as a Chronic Disease?
Weight Bias: Weight bias commonly results from not perceiving obesity as a medical condition. Efforts are made by organizations like the Obesity Action Coalition (OAC) to educate everyone regarding this unfair treatment of individuals affected by obesity.
Lack of Diagnosis: Despite being a medical condition, obesity is often omitted in a patient’s medical records. If it is not diagnosed, it will most likely not be treated. Healthcare providers need to make a conscious effort to remedy this.
Not Discussing Weight Concerns with Patients: In some instances, this may result from time constraints during medical visits. In others, lack of knowledge regarding obesity treatment prevents providers from starting this conversation. Dedicated obesity management visits by trained professionals are most appropriate to effectively treat obesity.
Not Utilizing Treatment Tools: This may be due to a lack of knowledge as well as misconceptions regarding safety of treatment options for obesity. Physician education regarding obesity treatment options is necessary.
Lack of Training: The number of providers seeking training in obesity management is increasing.
Lack of a Multidisciplinary Approach to Weight Management: As a complex medical condition, obesity requires a multidisciplinary approach. Nutritionists, behaviorists, exercise physiologists, bariatricians and surgeons all play a crucial role in providing individualized and comprehensive treatments of this complex and chronic medical condition.
Limited Access to Care: Fair access to obesity treatment options is necessary to allow for treatment – just like any other chronic medical condition. Efforts need to continue to improve our healthcare system.
Conclusion: In recent years, significant efforts have been made to understand obesity. It is now recognized as a medical condition. The next challenge is to successfully treat this complex, chronic and relapsing disease by identifying obstacles, improving treatment and improving access to care for anyone affected.
About the Author:
Nadia B. Pietrzykowska, MD, FACP, is a Board Certified and Fellowship trained Obesity Medicine and Nutrition Physician Specialist. She has a primary specialty in Internal Medicine. She is the Founder and Medical Director of “Weight & Life MD,” a Center dedicated to Medical Weight Management, Nutrition, Fitness and Lifestyle located in New Jersey. She strongly believes in a personalized as well as long-term approach to treating the chronic disease of obesity and its co-morbid conditions.
by Sarah Muntel, RD Spring 2024 Spring has sprung, bringing sunnier and warmer days! For many, this…
Read Articleby Yelena Kibasova Spring 2024 The fitness world is evolving, with new trends and innovations that promise…
Read Articleby Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read Article