Getting the Most out of Research About Bariatric Surgery

by David Arterburn, MD, MPH, and Jane Anau
Summer 2022
You’ve been wondering about bariatric surgery. When you first heard about it, you thought weight-loss was the only reason to have the surgery, so learning that bariatric surgery can be used to manage and treat your diabetes and hypertension was eye-opening. Treating these chronic health conditions is more important to you than weight-loss but you are worried about the risks of surgery. It’s a big deal, so you’ve taken your time to talk with your primary care doctor, and you’ve read real-life stories from people who had chosen to have or not have bariatric surgery. You’ve imagined the lifestyle changes you might need to make after surgery – will the outcomes be worth it? Is the cost of the surgery worth it? After reflecting on these ideas and talking with your family and friends, you’ve made the decision that surgery is right for you.
Choosing What’s Right for You
Now you face the next step – choosing which type of bariatric surgery to have. You’ve heard some people wish they’d chosen a different surgery, while other people remain happy with their choice.
It’s a big decision and you’re going to need the help of a surgeon to make it. There are so many things to consider with each procedure, it’s hard to know where to even start. Here are some questions you might be asking yourself:
- What can you do to prepare for a meeting with the surgeon?
- What kind of questions will he/she ask you?
- How should you answer?
- Will the surgeon help you understand the pros and cons of each procedure?
- What other resources are available that could help you with your decision-making?
Here’s a really important point to remember when planning your visit – there are no right answers and there is no “right” procedure. You and your surgeon enter the discussion with the same goal – to collaborate and make a decision about which type of surgery is right for you.
What Can I expect in my Appointment with a Surgeon?
Here’s what to expect in an appointment with a surgeon to consider different bariatric surgery procedure types:
- Your surgeon should make it clear that there is a decision to be made about what is the “right” procedure for you and that they want to help you make the best decision.
- Your surgeon should explain all the options available to you in plain language with information about risks, benefits, and uncertainties of the different operations. It’s expected that you may have questions, and you should ask them. This can help make sure you have the information you need to make a good choice.
- Your surgeon should engage you in a conversation about what is most important to you and discuss your treatment goals and concerns. You will talk together about how the different procedure choices align with your preferences.
One source of new research evidence that might help you in talking with your doctor comes from the PCORnet Bariatric Study (PBS), which is the largest long-term U.S. study on bariatric surgery to date. The study uses real-world data from 41 health organizations around the country to examine bariatric surgery results at 1, 3, and 5 years after surgery. Specifically, based on anonymous medical records from over 46,000 people who had bariatric surgery from 2005 to 2015, PBS compared different bariatric procedures in terms of weight-loss and regain, diabetes risk, and safety.
What are my Surgical Options?
There are several types of bariatric surgery, but the two most common operations are the gastric bypass and the sleeve gastrectomy.
- In gastric bypass, also called a Roux-en-Y (pronounced roo-en-wi) procedure, a surgeon uses part of the stomach to create a pouch that holds a small amount of food. The surgeon attaches this pouch to the small intestine. This procedure causes the body to absorb fewer calories.
- In sleeve gastrectomy, a surgeon removes a large part of the stomach, which limits the amount of food a person can eat.
Other bariatric operations are less commonly performed in the United States, including the adjustable gastric banding operation. Adjustable gastric banding is now less common because research shows better results and fewer long-term complications with gastric bypass or sleeve gastrectomy. For example, the PBS found that adults had more weight-loss with gastric bypass or sleeve gastrectomy than with adjustable gastric banding. Adults also had a higher chance of improvements in type 2 diabetes with gastric bypass or sleeve gastrectomy than with adjustable gastric banding. In addition, patients who had gastric banding had the highest risk of needing another surgery. For these reasons, the evidence below focuses on how sleeve gastrectomy compares to gastric bypass.
How Can These New Research Results Help You Prepare for the Appointment with Your Surgeon?
The PBS studied how gastric bypass and sleeve gastrectomy compare when it comes to weight-loss, effect on diabetes, and safety. The information below is based on the results of surgeries in adults aged 20 to 79 years old at the time of their surgery.
If your main concern is weight-loss, the PBS study found:
- Gastric bypass and sleeve gastrectomy are both effective in promoting large, durable weight-loss among adults. However, when compared head-to-head the gastric bypass procedure was the best option for losing weight and maintaining the weight-loss.
- People who had gastric bypass lost 31% of their weight in the first year and people who had sleeve gastrectomy lost 25%.
- At five years after surgery, people who received gastric bypass lost about 19 pounds more than people who had sleeve gastrectomy.
If your main concern is diabetes, our study found:
- Gastric bypass and sleeve gastrectomy are both effective at reducing the risk of diabetes but gastric bypass was slightly more effective in improving blood sugar levels long-term.
- With both gastric bypass and sleeve, diabetes went away, at least for some time, for most people with type 2 diabetes.
- For 86% of people who had gastric bypass and 84% who had sleeve gastrectomy, at some point in the 5 years after surgery, their records showed normal blood sugar and no prescriptions for diabetes medications.
- For some people, diabetes recurred after it went away.
- For people who had gastric bypass surgery, diabetes was slightly less likely to return than for people who had sleeve gastrectomy.
If your main concern is the safety of the surgical procedure, the PBS found:
- Bariatric surgery has a low risk of death. Overall, in our study, fewer than 1 in 100 people died—for any reason at all—within five years of either gastric bypass or sleeve gastrectomy surgery.
- Gastric bypass patients had a higher risk than sleeve gastrectomy patients of needing another operation or treatment related to their bariatric surgery.
- At five years after surgery, 12% of gastric bypass patients had a procedure related to their surgery compared to 9% of sleeve gastrectomy patients.
- Gastric bypass patients also had a higher risk than sleeve gastrectomy patients of other events such as hospitalization.
- People who have gastric bypass surgery risk more follow-up treatments because it is a more complex surgery than sleeve gastrectomy.
As you think about the information presented above, what seems most important to you? Is it the amount of weight-loss, the improvement in diabetes, or the risk of complications? Can you rank these in order of importance for you? Given what is most important to you, which operation appears to be best overall for that particular goal?
These questions can help you get closer to understanding what operation might be right for you, but you should still have a conversation with your surgeon. Every person is different, and your surgeon can help you to understand whether the results from the PBS study apply well to you – your individual health characteristics and your goals. Also, there might be other reasons why another procedure might be a good option. Having a conversation with your surgeon about the benefits and risks of the different operations, including data like those presented above, can help you make an informed choice that is guided by your own preferences, goals, and concerns. This can lead to better confidence in your decision-making and better satisfaction with your care long-term.
Summary
Information about weight-loss, diabetes risk, and the safety of the most common bariatric surgery procedures can help guide the conversation on procedure choice between you and your surgeon. Remember, there is no “right” choice. You and your surgeon can make a shared decision on which procedure is best for you. No matter what treatment options you are considering, we encourage exploring shared decision-making with a trusted medical professional.
Eligibility for the PBS
The PBS used anonymized and completely “de-identified” medical record data to study people who had bariatric surgery, including the following criteria:
- Individuals had to have had one of three bariatric procedures: Adjustable gastric band (AGB) – commonly known as lap band – Roux-en-Y gastric bypass (RYGB) – commonly known as bypass – and Sleeve gastrectomy (SG) – commonly known as sleeve.
- Their surgery happened between January 1, 2005, and September 30, 2015. It was required that the surgery was the first time the person had a bariatric surgery.
- Individuals had to have a BMI of ≥ 35 kg/m2 within a year prior to their surgery.
- Individuals who did not have cancer.
To learn more, please visit the following links for the PCORI Evidence Update for Patients:
www.pcori.org/evidence-updates/comparing-benefits-and-harms-bariatric-procedures
Funding Acknowledgement:
The PCORnet Bariatric Study was conducted in the National Patient-Centered Clinical Research Network, PCORnet. This study was funded by PCORI® via contract OBS-1505-30683. The views expressed in this article are solely the responsibility of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI), its Board of Governors or Methodology Committee. To learn more, please visit pcori.me/3BTbqeJ.
About the Authors:
David Arterburn, MD, MPH, FACP, FTOS, FASMBS (Hon) is a general internist and researcher at the Kaiser Permanente Washington Health Research Institute and Affiliate Professor with the University of Washington’s Department of Medicine in Seattle. He has published over 150 scientific papers on obesity, diabetes, and shared decision-making. The main focus of his current research is on identifying safe, effective, and affordable interventions to reduce the medical and psychosocial burden of obesity, with a special emphasis on the long-term outcomes of bariatric surgery.
Jane Anau, BS is a research project manager at the Kaiser Permanente Washington Health Research Institute. She works on studies related to bariatric surgery, diabetes, and persistent pain.
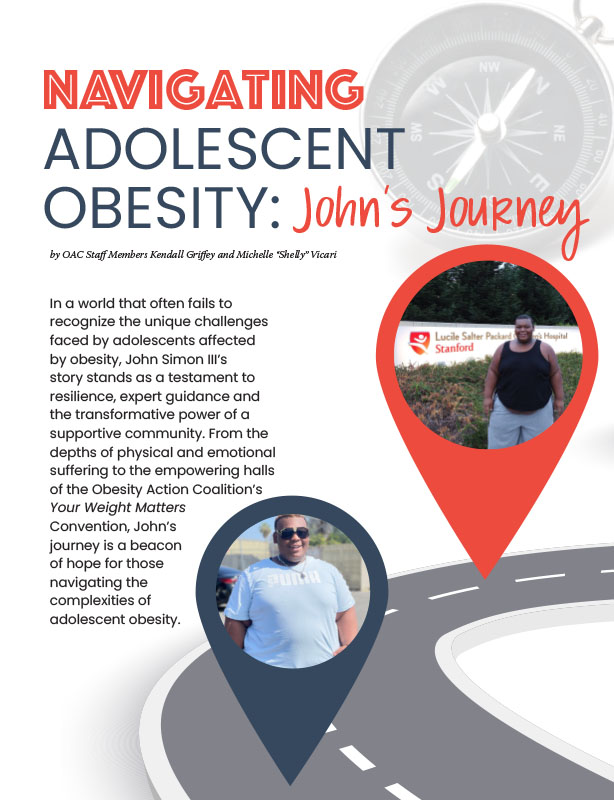
by OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read ArticlePost-operative addiction is often overly simplified as transfer addiction or cross-addiction, assuming individuals “trade” compulsive eating for…
View Video