Dear Doctor: Why Does Body Fat Cluster in Certain Areas?

by Scott Kahan, MD; and Adriana Williams, MD
Winter 2022
While we have some control over our weight such as changing what we eat and how much we exercise, other factors are outside of our direct control such as genetics, environment and social determinants of health. Where we gain weight is even less so in our direct control.
Why Does it Matter Where My Body Fat Clusters?
Typically, carrying more weight and storing too much fat increases health risks. And where we gain weight has an even greater impact on the risks for developing long-term health conditions including:
- Diabetes
- High blood pressure
- High cholesterol
- Heart disease
Fat accumulation is most common either in the midsection or the hips, thighs and buttocks. It is also important whether fat accumulates just under the skin (subcutaneous fat) or around the inner organs like the heart, liver and kidneys (visceral fat). Visceral fat has a greater impact on long-term health risks because these cells are more likely to make hormones and other chemicals that increase inflammation, blood clotting and overactive immune responses.
What is the Reason Fat Clusters in Certain Areas?
The areas of the body where fat clusters are primarily driven by the below factors:
- Genetics: About 50% of fat distribution is determined by genetics. Therefore, it’s likely that our weight will cluster in similar places as close relatives.
- Gender: Women usually have higher amounts of body fat than men and are more likely to accumulate fat in the hips and buttocks. This is believed to be an evolutionary development that allows for added energy storage for a developing fetus. Men, in contrast, tend to have more visceral fat, especially in the abdomen. This partly explains why men are at greater risk of developing diabetes and heart disease, among other long-term health conditions.
- Age: Over the years, body fat tends to increase, and visceral fat accumulation becomes more common. In part, this is due to changes in hormones over the latter decades of life.
- Hormones: Hormones can have a strong influence on weight and fat distribution. For example, as testosterone and estrogen decline in most people during the 40s and 50s, visceral fat is more likely to accumulate. In postmenopausal women, lower estrogen levels contribute to fat storage shifting from the hips and thighs toward the abdomen. Stress hormones such as cortisol also contribute to visceral fat storage.
In addition to the factors above, there are certain medical conditions and medications that can potentially impact where fat accumulates. For example, a medical condition such as lipedema may cause fat to accumulate in your lower body.
How Can I Measure My Body Composition?
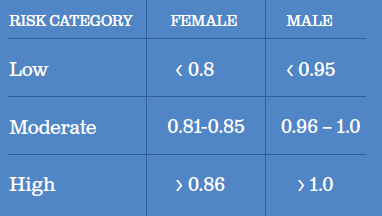
There are many ways to measure body composition, including expensive body scans, but in most cases, simple measurements are sufficient. Measuring waist-to-hip ratio is a quick way to estimate visceral abdominal fat vs subcutaneous lower body fat. Studies done by the Annals of Internal Medicine and Frontiers in Public Health have shown that people with higher waist-to-hip ratios are at greater risk for long-term health issues such as diabetes and heart disease. According to the World Health Organization, a high waist-to-hip ratio for men is 1.0 or greater and for women is 0.86 or greater.
Knowing This, What Can We Do?
First, let’s appreciate our bodies, regardless of weight, shape or size. From eyes and noses to skin and hair, to brains and fingerprints and personalities, we all look, feel and experience the world differently. We are each unique and have different shapes and sizes. Work hard to maximize your body’s health and abilities, but catch yourself before shaming its shape or size (or anyone else’s for that matter).
While we have little control over many of the factors discussed above, there are several things we can do to improve our health risks:
Minimize Sugary Foods
Foods that tend to spike insulin levels may increase the accumulation of visceral fat. Therefore, minimizing sugary foods and “junk foods” can lead to less visceral fat. In contrast, whole grains, complex carbs and lower-carb foods generally digest slower and don’t spike insulin levels as much.
Avoid Trans Fats and Saturated Fats
Additionally, trans fats and saturated fats may also increase the risk for belly fat. Unsaturated and polyunsaturated fats that are found in fish, nuts, seeds and vegetables can help reduce insulin resistance and visceral fat.
Be Active
Being active, regardless of weight, is one of the healthiest things we can do for ourselves. Physical activity improves insulin resistance, decreases visceral fat and reduces long-term health risks. Any kind of physical activity is beneficial. For some, exercising in the gym is preferred; for others, taking walks with friends or while listening to a podcast is more fun.
Both stress and sleep also impact visceral fat. Getting restorative sleep is especially important given that insufficient sleep impacts stress levels and metabolism. In one long-term study, those who slept too little (five or fewer hours per night) accumulated nearly three times as much visceral fat compared to people who slept 6-7 hours per night.
Conclusion
It’s important to pay attention to where your weight is clustering in your body because it could be affecting your health. If you are concerned about where your weight is clustering, be sure to consult with a healthcare provider about what you can do.
About the Authors:
Scott Kahan, MD, MPH, is a physician trained in clinical medicine and public health. Dr. Kahan is the Director of the National Center for Weight and Wellness in Washington, D.C. and Chair of the Clinical Committee for The Obesity Society. He serves on the Board of Directors for the OAC, the American Board of Obesity Medicine, The Obesity Society and the Obesity Treatment Foundation.
Adriana Williams, MD, is a Clinical Coordinator at the National Center for Weight & Wellness in Washington, D.C. She served as a Medical Assistant for the Institute of Neurological Recovery and was a medical student at Medical University Lublin.
by Kelli Richardson, RD You’ve probably heard the generic advice before: Eat your fruits and veggies. Limit…
Read Articleby Allen F. Browne, MD, FACS, FAAP, FOMA Summer 2023 “It’s not your fault!” These four words…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Article