Dear Doctor: My Child is Gaining Weight. How Do I Help Them?

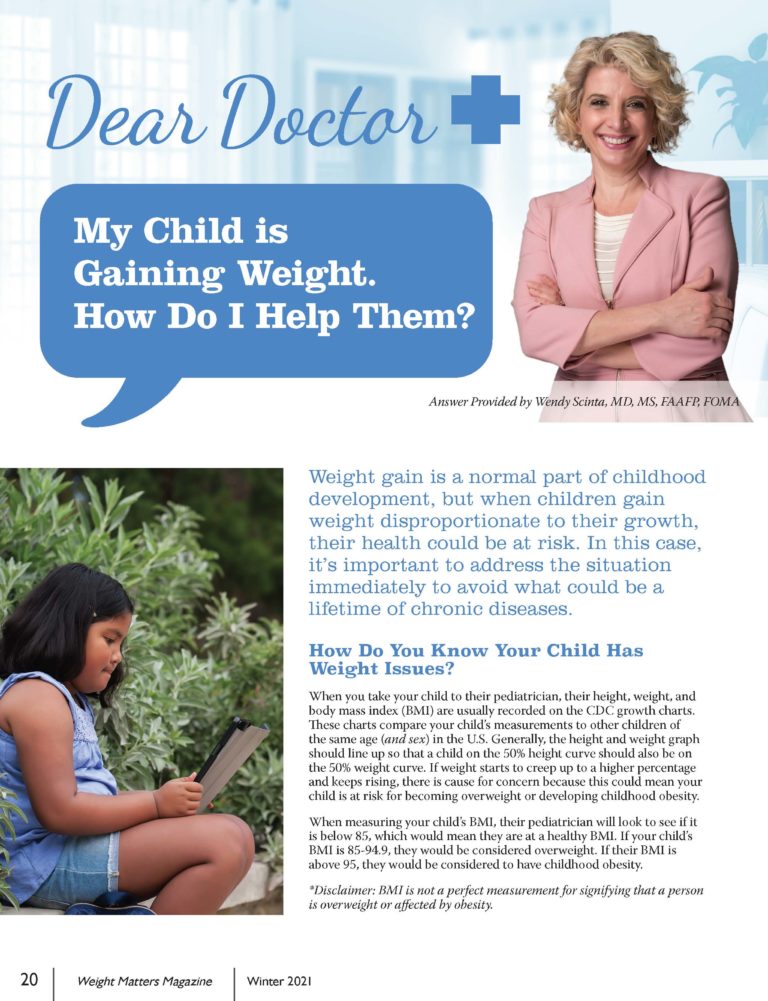
Answer Provided by Wendy Scinta, MD, MS, FAAFP, FOMA
Winter 2021
Weight gain is a normal part of childhood development, but when children gain weight disproportionate to their growth, their health could be at risk. In this case, it’s important to address the situation immediately to avoid what could be a lifetime of chronic diseases.
How Do You Know Your Child Has Weight Issues?
When you take your child to their pediatrician, their height, weight, and body mass index (BMI) are usually recorded on the CDC growth charts. These charts compare your child’s measurements to other children of the same age (and sex) in the U.S. Generally, the height and weight graph should line up so that a child on the 50% height curve should also be on the 50% weight curve. If weight starts to creep up to a higher percentage and keeps rising, there is cause for concern because this could mean your child is at risk for developing excess weight or childhood obesity.
When measuring your child’s BMI, their pediatrician will look to see if it is below 85, which would mean they are at a healthy BMI. If your child’s BMI is 85-94.9, they would be considered as having excess weight. If their BMI is above 95, they would be considered as having childhood obesity.
*Disclaimer: BMI has its limitations and is not a perfect measurement for assessing weight status. While it can be a helpful screening tool, it is not a measure of body fat and does not consider factors such as muscle mass, bone mass and fat distribution. Social determinants, race, ethnicity and age all modify the risk associated with a given BMI.
Medical Causes for Weight Gain
If your child’s BMI is in the childhood overweight or obesity range (greater than 85%), your child’s pediatrician may want to do a full work-up to rule out any medical causes for their weight gain. They will want to review your family’s medical history, rule out any genetic causes and review your child’s medications.
Family History
When being asked about your family’s medical history, you may be asked some of the following questions:
- Does anyone in your family have thyroid issues, diabetes or high blood pressure?
- What was the weight of the mother and father of the child when mom became pregnant?
- Were there any complications during pregnancy such as gestational diabetes or hypertension?
- What was the child’s birth weight?
- Did mom smoke during pregnancy?
- Was the child breast or formula fed?
Genetics
There are important (but rare) genetic causes of obesity that your child’s pediatrician or healthcare provider may want to rule out, particularly if that child is very young. These include:
- Prader-Willi Syndrome – This syndrome disrupts the hypothalamus in the brain, sometimes causing irregular hunger, body temperature, sleeping patterns and emotions.
- Bardet-Biedl Syndrome – A rare genetic disorder present at birth that can affect vision and kidney function and lead to weight gain.
- Cohen Syndrome – An inherited disorder that can cause intellectual disability, developmental delays and weak muscle tone.
- Alstrom Syndrome – A form of heart disease that can enlarge and weaken heart muscles, often causing obesity and diabetes.
- Congenital Hypothyroidism – A partial or complete loss of function in the thyroid that affects infants from birth.
Most of these health conditions are diagnosed shortly after birth but are very rare. However, it is important for your child’s pediatrician or other healthcare provider to rule them out when determining the cause of your child’s weight gain.
Medications
Sometimes, the medications a child is taking can cause them to gain weight. Weight gain is usually a symptom of:
- Medications used for depression, anxiety or mood disorders
- Steroids
- Hormones (for example, some birth control pills)
If you find that medication is a potential cause for weight gain, consult with your primary care physician before discontinuing the medication.
What If There Is No Medical Cause for Weight Gain?
While some cases of obesity in children are caused by genetics or other medical factors, some cases can be a result of food intake and physical activity. Obesity in children can be caused by what they eat, when they eat it, where they eat it and how much they eat.
When I am evaluating a child with weight issues, I ask the child and caregiver some questions:
- Is the child eating breakfast?
- Does he or she bring their lunch or buy at school?
- Is dinner in the car, out at a restaurant or at home?
- Does the family prepare meals together and eat at the table?
Going without breakfast, having frequent meals in the car or away from home, and eating fast food regularly all increase the chances that a child will struggle with a weight problem, possibly into their adult years if left unaddressed.
There are many things you can do at home to address your child’s weight in a healthy and sensitive way. I have found that many parents have no idea where to start, and by the time they make their way to my office, they are frustrated and hopeless. This is why I wrote the book, BOUNCE – A Weight-Loss Doctor’s Plan for a Happier, Healthier, and Slimmer Child. It gives parents or caregivers a starting point in how they can help their child.
Changes You Can Make at Home
There are some changes you can make as a family that will make a big difference right away. Consider implementing the following changes in your home:
- Limit time on digital devices.
- Limit eating out to no more than once per week.
- Refrain from all electronics while eating (cell phones, computers, television, etc.).
- Sit down to dinner as a family at least once per week.
- Model good behavior – your children are watching you!
- Remove negative food queues (such as bowls of candy or bags of chips) and present positive ones instead (such as a big bowl of fruit).
- Downsize plates and bowls (our brain likes to fill space).
- Eat breakfast – that means everyone!
- Don’t keep sugar-sweetened beverages in the home and limit your child’s consumption of them.
The BOUNCE Acronym
In my book, BOUNCE – A Weight-Loss Doctor’s Plan for a Happier, Healthier, and Slimmer Child, the BOUNCE acronym stands for:
Behavioral Modification: Working on eating behaviors that can cause weight gain.
Optimizing Metabolism: Eating breakfast and eating every three hours after to keep your metabolism going all day.
United as a Family: It is so important to make changes as a family and not to expect your child to follow different rules than his or her siblings or parents.
Notation of Food: It is important to record food and movement – not to count calories, but to help your child understand the value of the food they are eating, where it comes from, and how to make it better.
Counting Steps: This is the movement piece. Aim for 10,000 steps each day, but also record other activity as well and encourage exercise in a fun and healthy manner.
Elimination Diet: This involves looking at eating habits and slowly and mindfully replacing the unhealthy foods with delicious, healthier options.
Should My Child Be on Medication?
Continued weight gain can lead to orthopedic and metabolic issues including:
- High blood pressure
- High cholesterol
- Insulin resistance
- Metabolic Syndrome
- Pre-diabetes
- Diabetes
- Gallstones
- Kidney stones
- Fatty liver disease
- Vitamin deficiency
It’s important to note that if your child develops any of the above conditions, they are treatable with medications and some are reversible through weight-loss.
If your child’s pediatrician or other healthcare provider wants to start your child on medication for any of the above conditions, listen to their advice, but also take your child to a childhood obesity expert. A childhood obesity expert will implement a plan that includes nutritional and behavioral approaches, as well as physical activity, while treating their condition with medications that help promote weight-loss.
For more information about finding obesity experts in your area, visit ObesityMedicine.org or the OAC’s Provider Locator at ObesityCareProviders.com.
Conclusion
There are many ways to help your child manage their weight and improve their health. It’s important that your child doesn’t feel alone and that they are treated with understanding and compassion. Find your child a good pediatrician and partake in healthy eating and activities with them. The key to a healthier lifestyle is consistency and having an encouraging and helpful support system.
About the Author:
Wendy Scinta, MD, MS, FAAFP, FOMA, is a nationally-recognized expert in adult and childhood obesity treatment and is also the Immediate-Past President of the Obesity Medicine Association. She is a clinical assistant professor of family medicine at SUNY Upstate, Diplomat of the American Board of Family Physicians, and Diplomat of the American Board of Obesity Medicine. Dr. Scinta’s book, BOUNCE – A Weight Loss Doctor’s Plan for a Happier, Healthier and Slimmer Child, has been a bestseller in the field of childhood obesity, and her BOUNCE program has been implemented nationally and internationally.
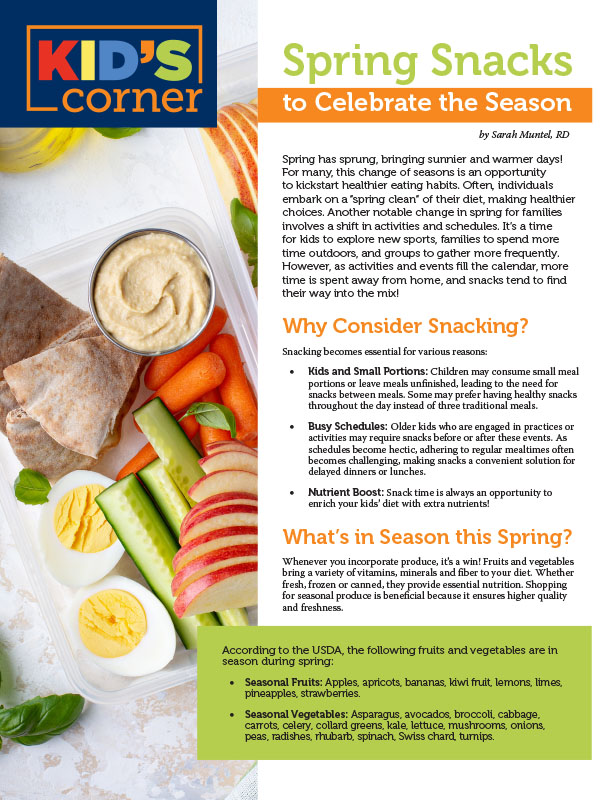
by Sarah Muntel, RD Spring 2024 Spring has sprung, bringing sunnier and warmer days! For many, this…
Read Articleby Yelena Kibasova Spring 2024 The fitness world is evolving, with new trends and innovations that promise…
Read Articleby Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read Article