Dear Doctor, I Think My Band Slipped. What are the signs?

Answer provided by Lloyd Stegemann, MD, FASMBS
Spring 2013
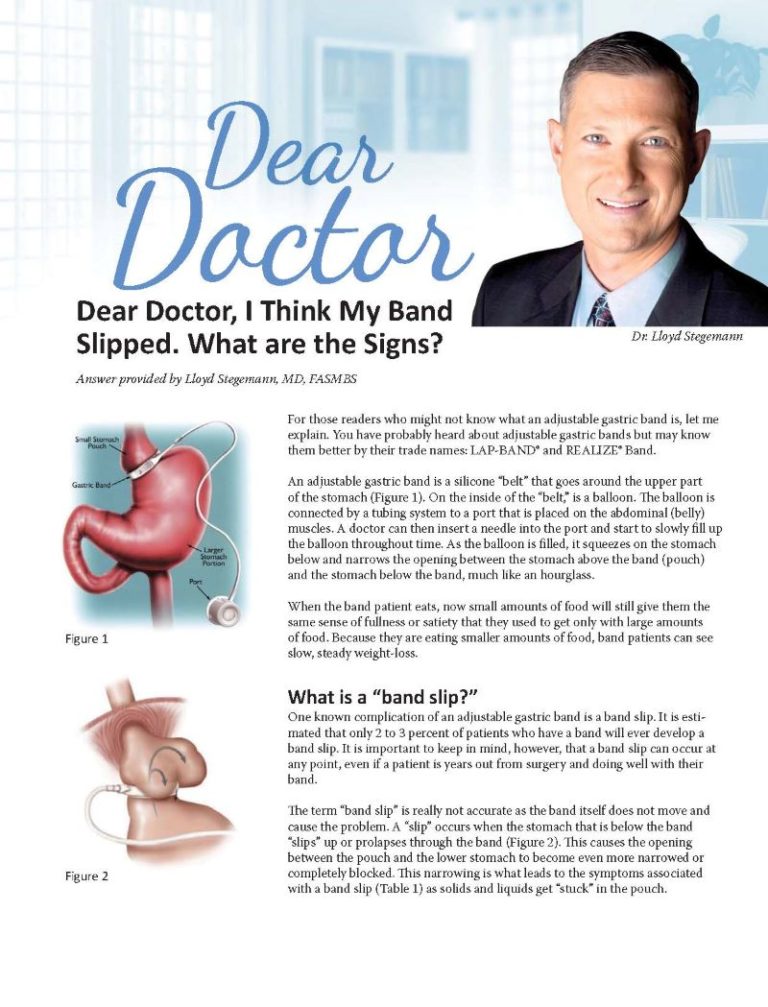
For those readers who might not know what an adjustable gastric band is, let me explain. You have probably heard about adjustable gastric bands but may know them better by their trade names: LAP-BAND® and REALIZE® Band.
An adjustable gastric band is a silicone “belt” that goes around the upper part of the stomach (Figure 1). On the inside of the “belt,” is a balloon. The balloon is connected by a tubing system to a port that is placed on the abdominal (belly) muscles. A doctor can then insert a needle into the port and start to slowly fill up the balloon throughout time. As the balloon is filled, it squeezes on the stomach below and narrows the opening between the stomach above the band (pouch) and the stomach below the band, much like an hourglass.
When the band patient eats, now small amounts of food will still give them the same sense of fullness or satiety that they used to get only with large amounts of food. Because they are eating smaller amounts of food, band patients can see slow, steady weight-loss.
What is a “band slip?”
One known complication of an adjustable gastric band is a band slip. It is estimated that only 2 to 3 percent of patients who have a band will ever develop a band slip. It is important to keep in mind, however, that a band slip can occur at any point, even if a patient is years out from surgery and doing well with their band.
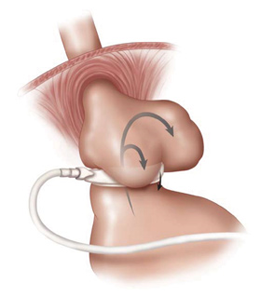
The term “band slip” is really not accurate as the band itself does not move and cause the problem. A “slip” occurs when the stomach that is below the band “slips” up or prolapses through the band (Figure 2). This causes the opening between the pouch and the lower stomach to become even more narrowed or completely blocked. This narrowing is what leads to the symptoms associated with a band slip (Table 1) as solids and liquids get “stuck” in the pouch.
Symptoms of a Band Slip
1. Severe heartburn or reflux (GERD)
2. Pain when eating solid food (dysphagia)
3. Vomiting with solid foods
4. Night cough
5. Chest pain or pressure
If a band patient experiences any of these symptoms, they really need to be evaluated by their surgeon. If a band patient suddenly finds that they are vomiting all solids and liquids, vomiting saliva or having chest/abdominal pain that won’t go away, they need to be seen immediately. Large slips can cause the blood supply to the stomach below the band to be cut off and are a true surgical emergency! Luckily most slips are small and don’t require emergency treatment.
What happens if I have a band slip?
If your surgeon suspects you have a slip, they will usually order a radiology test called an upper GI. You will be asked to drink some nasty tasting fluid (barium) and a radiologist will snap some pictures of the fluid going down your esophagus and into the pouch. By looking closely at the pouch, your surgeon will be able to see if there is a slip and if there is, how big is the slip.
Depending on the size of the slip, your surgeon will decide the best therapy. Sometimes just taking fluid out of the band will allow the stomach that slipped up to return to where it was before. unfortunately, this isn’t always the case and some band slips may require an operation to reposition the band.
If a patient has a repair of a band slip and they ultimately have another slip, most surgeons would recommend having the band removed. Luckily, band slips don’t happen often; however, when they do, it can be serious. If you have a band and are concerned about having a slip, it’s always best to get it checked out by your bariatric surgeon.
Answer provided by:
Lloyd Stegemann, MD, FASMBS, is a private practice bariatric surgeon in Corpus Christi, TX. He is the driving force behind the Texas Weight-loss Surgery Summit and the formation of the Texas Association of Bariatric Surgeons. Dr. Stegemann is a member of the American Society for Metabolic and Bariatric Surgery, OAC National Board of Directors, Co-chair of the Convention Program Agenda Subcommittee and is Chair of the OAC Sponsored Membership Program.
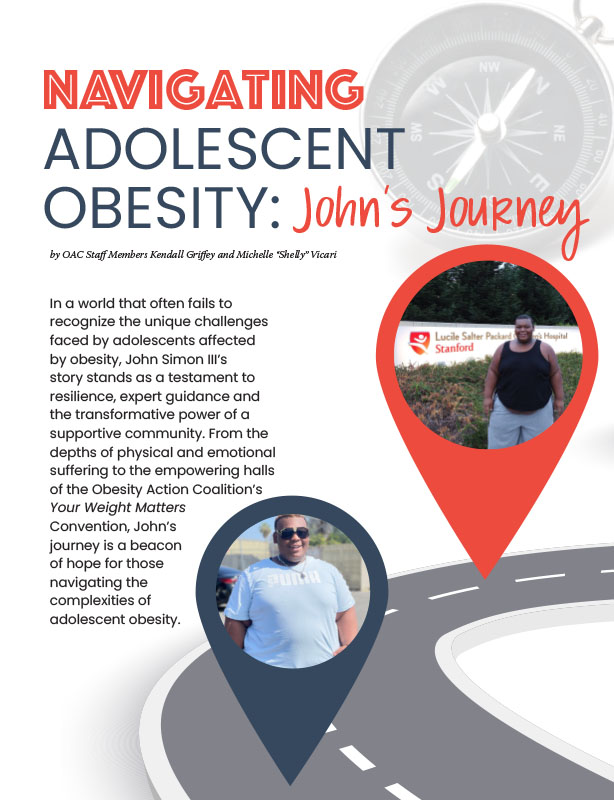
by OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read ArticlePost-operative addiction is often overly simplified as transfer addiction or cross-addiction, assuming individuals “trade” compulsive eating for…
View Video