Dear Doctor, How Do I Choose the Right Bariatric Surgery Procedure for Me?

Answer Provided by Lloyd Stegemann, MD, FASMBS
Spring 2018
Throughout the last decade, America’s obesity epidemic has continued to get worse. Recent U.S. data shows nearly 40 percent of Americans have severe obesity, with even higher rates in women and minorities. Along with this weight, significant medical problems arise such as high blood pressure, diabetes, sleep apnea, heart disease and several types of cancer.
For those with severe forms of obesity (BMI >40), bariatric surgery has been shown to be the most reliable method for achieving long-term weight-loss and improvement in weight-related medical problems. Throughout the past 10 years, the risk of having these procedures has continued to decrease due to improvements in care before, during and after surgery. Today, the average risk patient having a bariatric operation is at no greater risk than if they were having their gallbladder removed! For these reasons, more and more individuals with obesity are looking to bariatric surgery as a treatment option.
Before You Choose to Have Bariatric Surgery
To save you time and possible disappointment, there are a number of considerations and some legwork that should be done before you make an appointment with a bariatric surgery program. Here are a few things to consider:
- Are you at a place in your life where you have the time and ability to dedicate the required effort after surgery to be successful? Because of safety improvements, actual surgery is the easy part for most patients. The real work starts after surgery as you begin creating the healthy habits necessary for maximizing the results of your operation. This means making significant changes in your life that can bring about stress and turmoil if not handled properly. I recently saw a patient who was a mother of three school-age kids, worked a full-time job and went to school at night – all while trying to maintain her home and family life. It was clearly not a good time for her to consider bariatric surgery.
- Does your health insurance cover bariatric surgery? While the bariatric surgery program you choose will check this for you, it is helpful to know this information before you call the program. The easiest way to get this information is to call your insurance company, but there are other ways as well. Do you have a Human Resources Department at your job? Do you have the same plan as co-workers that have had bariatric surgery? If your insurance plan does not cover bariatric surgery, you will have to decide if you have the ability to pay cash for your operation. There are a number of options for getting the money to pay for surgery, including getting a loan from a medical financing company, taking out a home equity loan, borrowing from a 401K or borrowing from a family member.
- Do you have the finances to cover out-of-pocket costs before bariatric surgery? Most patients can expect to pay somewhere between $2,000-4,000 before their operation to cover costs of pre-operative tests, labs, surgeon fees, anesthesia fees and hospital fees.
- Do you have paid time off available at your job? In general, people will miss two weeks of work after bariatric surgery – but this is variable.
Finding Your Bariatric Surgeon/Program
Once you have answered these questions, it’s time to look for a bariatric surgery center in your area. The easiest way to do this is to visit the American Society for Metabolic and Bariatric Surgery (ASMBS) website at ASMBS.com and use the “Find a Provider” feature. After entering your zip code, you will see all of the bariatric surgeons in your area along with their contact information.
Once you get this information, I would encourage you to do the following:
- Research the surgeon’s website, Facebook page, Twitter profile, etc. to learn more about them and the program they offer. Do they offer all bariatric surgery options, or do they just do one type of surgery? How long have they been performing bariatric surgery? Do they operate at a hospital that is accredited in bariatric surgery? Who covers for them when they are unavailable? Do they offer an aftercare program?
- Research online to see what other patients are saying about the surgeon or their program.
- Talk to other patients who used that surgeon and ask about their experience before, during and after surgery. How is the surgeon’s bedside manner? Is the office easy to work with? Are calls returned promptly?
- Consider going to a support group meeting to meet others who used that program.
Choosing Your Procedure
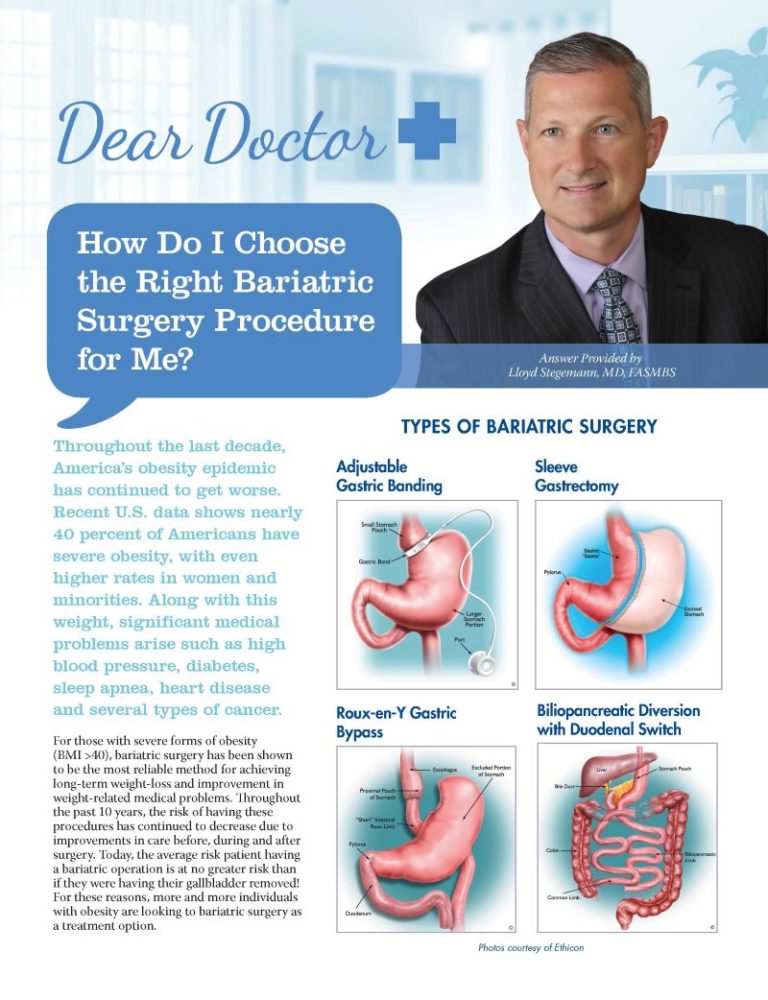
Here are the most common bariatric operations and the percentage they make up of the total bariatric operations performed in 2016:
- Sleeve Gastrectomy – 58.1 percent
- Gastric Bypass – 18.7 percent
- Gastric Band – 3.4 percent
- Duodenal Switch – 0.6 percent
Most patients “know” which surgery they want to have when they come to their first appointment. This is usually based on the fact that they have a friend, colleague or family member who has had success with a particular bariatric procedure. Other times, they’ve heard “bad things” about another procedure.
It’s important to keep an open mind when considering the different options available to you, because there is a lot of misinformation out there that can sway you toward an operation which might not be in your best interest. There is no “right” operation for everybody. All of the available bariatric operations are effective, but there are certainly differences between them.
Here are some things that should be considered when choosing the “right” procedure for you:
Risk Tolerance
While every operation has risk of complication and the possibility of death, some operations carry more risk than others. For bariatric surgery, the risk of complication and death in the first 30 days after surgery from least risky to riskiest is:
- Gastric Band
- Sleeve gastrectomy
- Gastric bypass
- Duodenal switch
The risk of complication or death often depends on a number of factors, including the medical condition of the patient prior to surgery and surgeon experience with different procedures. When you meet with your surgeon, they can give you a better idea of your individual risk.
Amount of Weight You Want to Lose
Each of the bariatric operations has a different amount of total body weight that a patient can expect to lose within 12-18 months after surgery.
- 25 percent with gastric band
- 30 percent with a gastric sleeve
- 35 percent with gastric bypass
- 40 percent with duodenal switch
It’s important to keep in mind that these are averages, so some patients will lose more and some will lose less than the predicted amount. In my experience, gastric bypass and duodenal switch patients almost always lose the predicted amount of weight – but sleeve and band patient results are much less predictable. This is likely because gastric bypass and duodenal switch operations create a stronger “metabolic effect” in the body when compared to the sleeve gastrectomy and band. If a patient would like to lose more weight than the amount predicted with their chosen procedure, they should strongly consider medical weight management before bariatric surgery.
Ability to Follow-up
While follow-up is important for success after every bariatric surgery, it’s especially true for the band and duodenal switch. If the band is not adjusted on a regular basis during the first two years after surgery, the patient will see minimal success. This means the patient will need to come in for regular visits (usually monthly for the first year). If the patient lives a long distance from the center, has difficulty getting time off work, can’t afford copays or their band fills, then the band is very unlikely to produce the results they are looking to achieve.
Of the stapled procedures (sleeve, bypass, duodenal switch), the duodenal switch patient has the greatest chance of developing life-altering vitamin and mineral deficiencies or malnutrition. Therefore, they need their labs checked regularly – especially during the first year after surgery.
Eating Habits and Lifestyle
To be successful after surgery, patients must work on changing their eating habits. This means focusing more on proteins and vegetables and less on carbohydrates, sweets and liquid calories.
All bariatric operations help reduce hunger and improve portion control. With the gastric bypass and duodenal switch, the operation also helps reinforce healthier eating habits by creating negative effects (nausea, abdominal pain or diarrhea) when the patient eats too much sugar or fat. This negative feedback often helps patients adapt to a healthier diet if they’ve previously struggled controlling their sweet and fat intake.
The gastric bypass operation also seems to decrease sweet cravings more than other operations. Duodenal switch patients will often have five to seven watery bowel movements a day in the early months after surgery, but this will ultimately shift to four to five formed bowel movements. This does not occur with the band, sleeve or gastric bypass.
Medical Conditions
There are certain medical conditions that, when present, would favor one operation over another. A full discussion of this topic is out of the scope of this article, but examples include diabetes, hiatal hernia, gastroesophageal reflux disease (GERD), Crohn’s Disease, kidney failure, smoking, arthritis, steroid dependence and multiple abdominal operations.
Reversibility/Revise Ability
While every bariatric operation should be considered “permanent” and there are very few reasons why one would be reversed, it is possible to take out a band and reverse a gastric bypass (put the pieces back together).
Because a large portion of the stomach is removed with a gastric sleeve and a duodenal switch, it is not possible to reverse these operations. On the other hand, if a band patient or a sleeve patient doesn’t achieve the desired weight-loss and improvement in weight-related medical problems, these operations can be revised to a different bariatric operation. It would be quite unusual to see a gastric bypass or duodenal switch patient revised to a different bariatric operation.
Conclusion
Bariatric surgery is a safe, effective way to achieve sustained weight-loss, improvement in weight-related medical problems and improved quality of life. However, there is no way to predict with any certainty what the “right” bariatric operation for any particular patient is. Doing your homework before seeing your surgeon and choosing the operation that best fits your weight-loss goals, risk tolerance and lifestyle will guarantee you get the “right” bariatric operation for you.
About the Author:
Lloyd Stegemann, MD, FASMBS, is a bariatric surgeon in Corpus Christi, Texas. Dr. Stegemann is a passionate advocate for universal access to bariatric surgery and is a former National Board Member of the OAC.
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
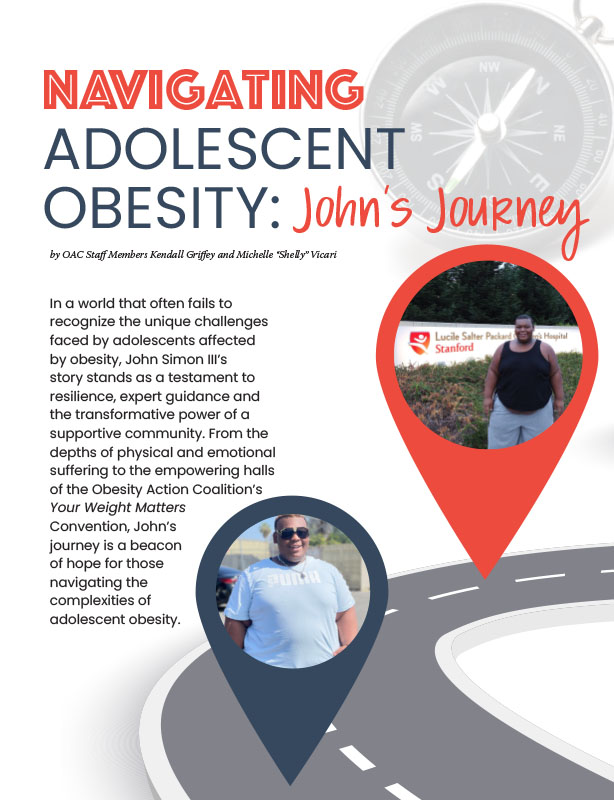
Read Articleby OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Article