Dear Doctor: How Can We Help the Obesity Epidemic?

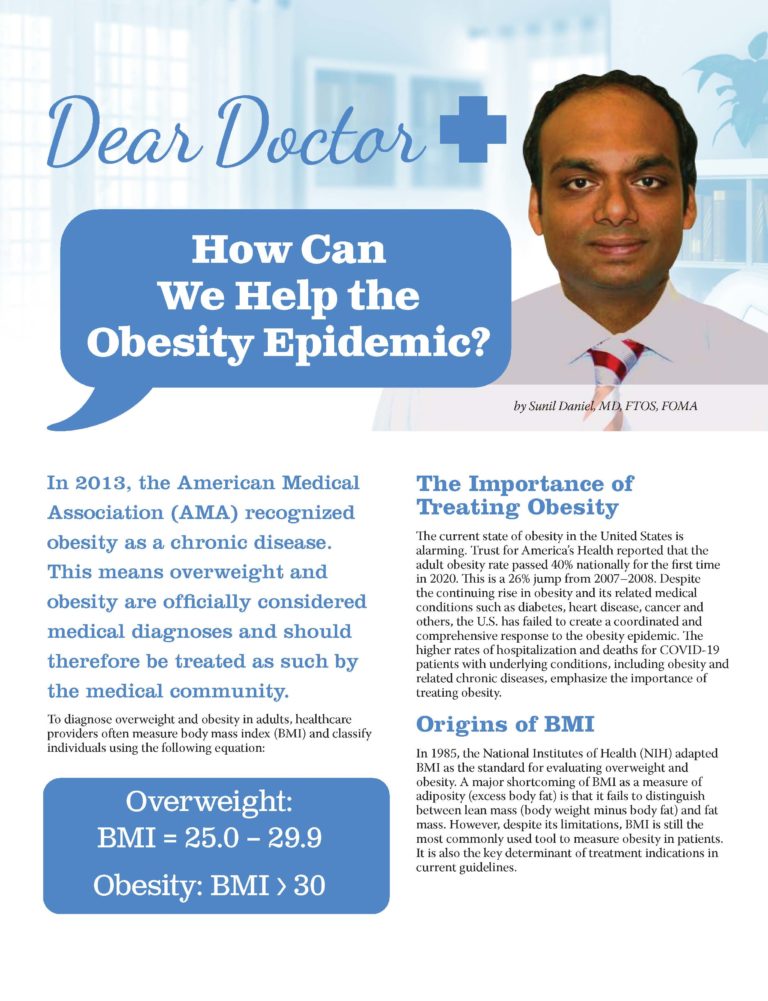
by Sunil Daniel, MD, FTOS, FOMA
Winter 2023
In 2013, the American Medical Association (AMA) recognized obesity as a chronic disease. This means overweight and obesity are officially considered medical diagnoses and should therefore be treated as such by the medical community.
To diagnose overweight and obesity in adults, healthcare providers often measure body mass index (BMI) and classify individuals using the following equation:
Overweight: BMI = 25.0 – 29.9
Obesity: BMI > 30
The Importance of Treating Obesity
The current state of obesity in the United States is alarming. Trust for America’s Health reported that the adult obesity rate passed 40% nationally for the first time in 2020. This is a 26% jump from 2007–2008. Despite the continuing rise in obesity and its related medical conditions such as diabetes, heart disease, cancer and others, the U.S. has failed to create a coordinated and comprehensive response to the obesity epidemic. The higher rates of hospitalization and deaths for COVID-19 patients with underlying conditions, including obesity and related chronic diseases, emphasize the importance of treating obesity.
Origins of BMI
In 1985, the National Institutes of Health (NIH) adapted BMI as the standard for evaluating overweight and obesity. A major shortcoming of BMI as a measure of adiposity (excess body fat) is that it fails to distinguish between lean mass (body weight minus body fat) and fat mass. Additionally, social determinants such as race, ethnicity and age may modify the risk associated with a given BMI. However, despite its limitations, BMI is still the most commonly used tool to measure obesity in patients. It is also the key determinant of treatment indications in current guidelines.
The New Model for Prevention and Treatment of Obesity: ABCD
Obesity is a complex disease that involves more than just an increase in body mass. The conventional diagnosis of obesity, based on BMI, is an indirect measure of body mass and provides no information about the effects of excess weight on health.
New models and guidelines proposed by societies such as the American Association of Clinical Endocrinology (AACE) use a complication-centric approach to manage obesity. According to a new article in the scientific community about treating obesity, obesity is now also referred to as Adiposity Based Chronic Disease (ABCD).
There are two ways to measure Adiposity Based Chronic Disease (ABCD):
- Screening and diagnosing ABCD using physical measurements such as height and weight
- Screening for the presence and severity of health complications such as diabetes, heart disease, liver disease, sleep apnea, etc.
Many people suggest that ABCD is a more precise clinical model for treating obesity. This way of thinking highlights the fact that the goal of obesity treatment shouldn’t just be weight-loss, but also the prevention and treatment of medical complications to improve overall health and quality of life.
Common Health Effects of Overweight and Obesity
According to the Centers for Disease Control (CDC)
- Type 2 diabetes
- Sleep apnea
- High blood pressure
- High LDL (bad) cholesterol
- Low HDL (good) cholesterol
- Stroke
- Coronary heart disease
- Different types of cancer
- Osteoarthritis
- Gallbladder disease
Why and How to Treat an Elevated BMI:
Primary Prevention:
Goal: To intervene before health is worsened. Getting a vaccination and developing healthy habits, such as balanced eating and regular exercise, are examples of primary prevention.
Primary prevention for ABCD includes:
- Public health messaging
- Changes in our built environments (such as sidewalks and parks)
- Promoting healthy lifestyles
- Providing access to preventive health care
- Providing access to maternal-fetal health
Those at increased risk of ABCD because of genetics (such as having a strong family history of obesity) may require a more targeted and personalized approach for lifestyle habits that support a healthy weight.
Secondary Prevention:
Goal: To screen and identify diseases in their earliest stages before the onset of signs and symptoms. Screening tools include measuring BMI, measuring blood pressure, and getting bloodwork done.
With the development of overweight and obesity, secondary prevention efforts must prevent further weight gain and screen for/monitor health complications such as high blood pressure, high blood sugar, acid reflux, sleep apnea and others. The presence of prediabetes, metabolic syndrome, high cholesterol, pre-hypertension and/or fatty liver indicates the presence of insulin resistance and cardiometabolic disease. Individuals with these conditions are at increased risk of one or all of the end-stage complications of cardiometabolic diseases, such as:
- Congestive heart failure
- Stroke
- Hypertension
- Type 2 diabetes
- NASH
- Chronic kidney disease
A weight-loss of just 7-10% is often enough to prevent these complications.
Tertiary Prevention:
Goal: To reduce the effects of ABCD once established.
Once complications from ABCD occur and advance, more aggressive weight-loss is required to manage them. In patients with type 2 diabetes, the more weight-loss they achieve, the better. Losing just 5-15% of your total body weight can improve blood sugar, blood pressure and cholesterol levels. For obstructive sleep apnea, a weight-loss of at least 10% is generally needed to see noticeable improvements. A weight-loss of 5-10% is needed to improve nonalcoholic fatty liver disease. Overall, losing 10-20% of your total body weight is required to improve weight-related medical complications in patients with ABCD.
Working with Your Doctor
ABCD is not currently curable and requires lifelong treatment and follow-up care. Lifestyle interventions and obesity medications can be extremely helpful. However, results generally aren’t permanent because of our complex biology.
Bariatric surgery procedures can help counter our complex biology. However, few patients attain their ideal body weight, many regain weight, and all require long-term follow-up care to manage their obesity. Therefore, clinicians and patients should be committed to the long-term treatment of ABCD with the goal of achieving sufficient weight-loss to optimize health by preventing and treating its complications.
Also, clinicians and patients must understand that weight-loss is not the only important factor in the obesity epidemic. Many patients experience weight stigma, shame, guilt and hopelessness.
Attempts to lose weight are frustrating at times, both for patients and clinicians. Treating each patient with respect, offering attention and support, and developing individualized treatment approaches are all important to making progress and improving health.
About the Author:
Sunil Daniel, MD, FTOS, FOMA, is a board-certified obesity medicine physician with fellowship training in clinical nutrition and obesity management. He is a fellow of The Obesity Society (TOS) and Obesity Medicine Association (OMA) and has authored several scientific papers on obesity and its medical management. He is also an Obesity Action Coalition (OAC) National Board Member and serves on the Education Committee.
by Sarah Muntel, RD Spring 2024 Spring has sprung, bringing sunnier and warmer days! For many, this…
Read Articleby Robyn Pashby, PhD Winter 2024 “No one is ever going to date you if you don’t…
Read Articleby Michelle “Shelly” Vicari Winter 2024 Winter has arrived! Don’t allow the chilly and damp weather to…
Read Article