Dear Doctor- Can You Cure My Obesity?

Answer Provided by Sunil Daniel, MD, FTOS
Summer 2018
In 2013, the American Medical Association (AMA) recognized obesity as a chronic disease. This means overweight and obesity are medical diagnoses and should be treated as such. To diagnose overweight and obesity in adults, healthcare providers often measure body mass index (BMI) and classify individuals using the following guidelines1:
- Overweight: BMI = 25.0 – 29.9
- Obesity: BMI > 30
So, what does this mean? A chronic disease such as obesity, diabetes, heart disease or arthritis lasts for a long time. It can’t be prevented by vaccines or cured by medications, and it actually becomes more common with age. In 2014, 61 percent (approximately 189 million) of Americans ages two and above were either classified as having overweight or obesity. The rate of obesity continues to increase!
Obesity over Time
Over time, the human body has evolved to save excess energy (or calories) as fat. Excess fat results in obesity, which often produces the following consequences:
- Elevated blood pressure, bad cholesterol and triglycerides
- Lowered good cholesterol, increased risk for type 2 diabetes, liver disease, joint pain and sleep apnea, and increased risk for a variety of cancers (more than 50 are associated with obesity)
Thankfully, within the last 20 years, there has been significant improvement in our understanding of obesity, its causes and why it’s so difficult to lose and maintain weight5. Treatment options for obesity include:
- Lifestyle modification (with nutrition, physical activity and behavior components)
- Medications
- Bariatric surgery
Lifestyle modification and medications are successful at delivering 5-10 percent weight-loss, which helps to prevent or manage obesity’s associated conditions. However, maintaining this weight-loss can be challenging over the long-term. It’s often reported that people who initially lose weight will regain some of it, or all, within a few years.
So, What Causes Obesity?
Obesity is a complex disease and body weight is affected by many factors. Some of the greatest factors include energy balance (calories in, calories out), environment, biology, genetics, medications and behavior. Let’s briefly discuss each of these below.
Energy Balance:
In the past, poor habits, unhealthy eating and large portions were considered to be the main causes of gaining excess fat2. We now understand the concept of energy balance within the body which is controlled mostly by the brain. When energy (food) intake is matched to energy output (metabolism and exercise), the size of the body’s energy stores (fat mass) is stable and no excess body fat is created.
When we eat more than we need, extra energy is stored as excess body fat. Over time, overeating can lead to weight gain and obesity. However, energy balance is not just eating and movement. It is also influenced by other factors such as environment, genetics, biology, medications and eating for reward or pleasure. Therefore, to lose weight, we need to reduce the amount of calories we consume and address other factors that may be influencing weight gain.
Environment:
In nations like the United States, food has become plentiful and is available around the clock. Food has also become social. We not only eat for survival, but also for enjoyment and amusement4. In addition, activity levels have decreased over time. As a result, we need fewer calories today than people needed 50 to 100 years ago. However, as a society, we’ve increased our caloric intake.
Existing public policies concerning food and health were developed decades ago and need to change in order to adapt to our current environment. Also, the food industry offers what consumers generally eat and drink but is overrun with options high in fat and calories and low in nutritional value. Active transportation such as walking and biking are helpful in weight regulation, but our most common mode of transportation is by automobile and safe walking and biking paths can be hard to find.
Finally, culture, bias and discrimination all play an important role that can’t be ignored! Bias and discrimination affect a large number of people in all areas of life – including employment, education and healthcare.
Biology:
Our body weight, energy balance and drive to eat form complex communication between our brain, gastrointestinal (GI) tract and other organs.
There are two brain pathways we need to consider:
- One that drives hunger
- One that drives fullness
Each pathway is also associated with hormones. When our weight is stable, our brain and stomach communicate effectively to determine food availability, hunger and fullness from meal to meal in order to maintain that weight. When these systems aren’t working correctly, this can lead to overeating and result in weight gain.
Genetics:
A gene is a trait (hair color, height, etc.) passed from parents to children. We have more than 20,000 genes in our body – some of which can determine if you are at greater risk for having excess weight or obesity. Like all causes of obesity, how genetics affects obesity is complex. Factors such as environment, biology and lifestyle affect genetics as well.
Many studies confirm that genetics affects BMI within a family. But it’s not just about genetics! Studies show a 55 percent difference in genes that affect body fat (passed from parents to children), while there is a 35 percent additional difference from factors (like environment) that affect body fat3. Current knowledge supports a strong genetic link between BMI, body fat and obesity, but we need additional research to clearly show the link between genetics and biology as well as behavior and lifestyle.
Medications:
When these systems aren’t working correctly, this can lead to overeating and result in weight gain. Some of those include medications to treat type 2 diabetes, steroid hormones, antidepressants, antipsychotics and medications for reducing hypertension. While this is not a reason to stop taking these medications, it’s important to be aware of potential side effects.
Behavior:
Food provides us with more energy to get through the day. It also gives us pleasure and reward. Part of our brain is sensory; it controls sight, smell and taste. It tells us when we eat something we like. We are conditioned to eat our trigger foods (chocolate, salty/crunchy snacks and sweets) by cues, triggers and even memory! Humans have the ability to make conscious choices, but powerful chemicals in our brain can heavily influence those decisions and make us feel good after eating foods high in fat and sugar. When we crave and eat these foods frequently, we gain weight.
What Happens When We Lose Weight?
Average weight-loss of 5-10 percent is generally set as a goal because that amount has been shown to produce clinically significant health improvements5. Despite current advances in treatment, weight regain after weight-loss remains a difficult problem. Weight management is a life-long process for nearly all Americans
no matter their current weight.
Behavioral or lifestyle modifications (a combination of diet, exercise and mental strategies) are usually needed for permanent weight-loss – either alone or combined with anti-obesity medications5. However, challenges with this approach exist, including sticking to the plan long-term and figuring out how each individual responds to treatment. Biological or physiological challenges include changes in our body which encourage weight gain – including lowered metabolism, increased hunger and decreased fullness. Finally, our general preference for tasty, high-energy foods plays a role in weight management.
A major clinical study which examined long-term weight management found that hormone changes encourage weight regain after weight-loss that has been achieved through diet. It also found that changes don’t return to normal values even 12 months after the initial weight-loss6.
Another study that followed contestants from the television show “The Biggest Loser” found that almost all participants regained a substantial amount of weight within the first six years after the competition. However, they were overall quite successful with long-term weight-loss compared to other lifestyle interventions. But even with weight regain, a large decrease in metabolic rate was seen – and those with greater long-term weight-loss also had greater slowing of the metabolism over time. Therefore, long-term weight-loss requires us to be constantly alert in order to combat these types of changes7.
Conclusion
What does all of this mean? Obesity cannot be cured or defeated because it’s a chronic disease. However, there is hope for sustained weight-loss. The National Weight Control Registry (NWCR) has provided evidence and specific strategies for achieving and maintaining weight-loss. They’ve also identified lifestyle modifications practiced by successful individuals which we have listed
on this page8.
These are key characteristics of those who have successfully maintained weight-loss:
- A continued low-calorie diet with high levels of physical activity
- Regular self-monitoring of food intake and exercise
- Eating breakfast every day
- Regular self-monitoring of weight (once a week or more frequently)
- Watching less than 10 hours of television per week
- Exercising an average of one hour per day
- Consuming low or no-calorie sweetened beverages
It is important that both healthcare providers and patients are aware of this information. Being knowledgeable and receiving appropriate support during their long-term weight management journey can make them more successful!
About the Author:
Sunil Daniel, MD, FTOS, is a board certified obesity medicine physician with fellowship training in clinical nutrition and obesity management. He is a fellow of The Obesity Society and has authored several scientific papers on obesity and its medical management. He also serves on the OAC Education Committee.
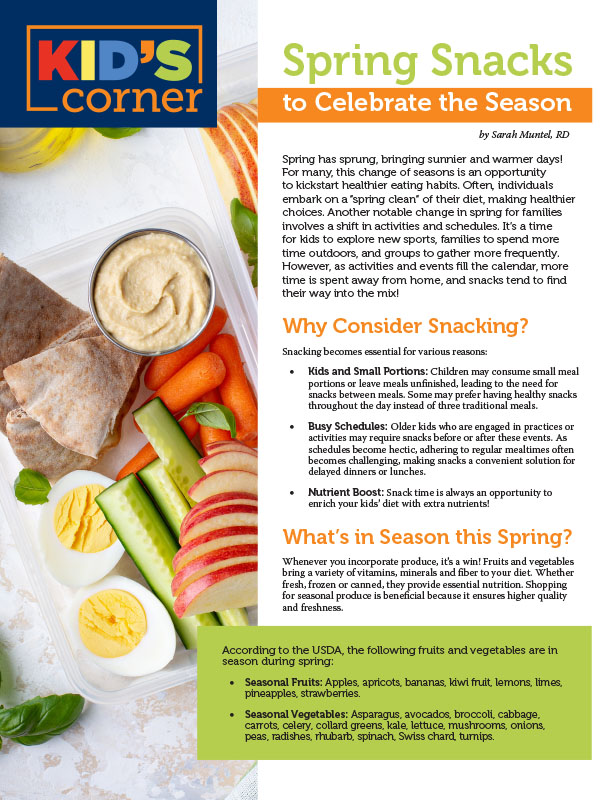
by Sarah Muntel, RD Spring 2024 Spring has sprung, bringing sunnier and warmer days! For many, this…
Read Articleby Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read Articleby Nina Crowley, PhD, RD (with Inspiration from Shawn Cochran) Winter 2024 Dating, no matter your age,…
Read Article