Dear Doctor: Can losing weight too fast hurt me?

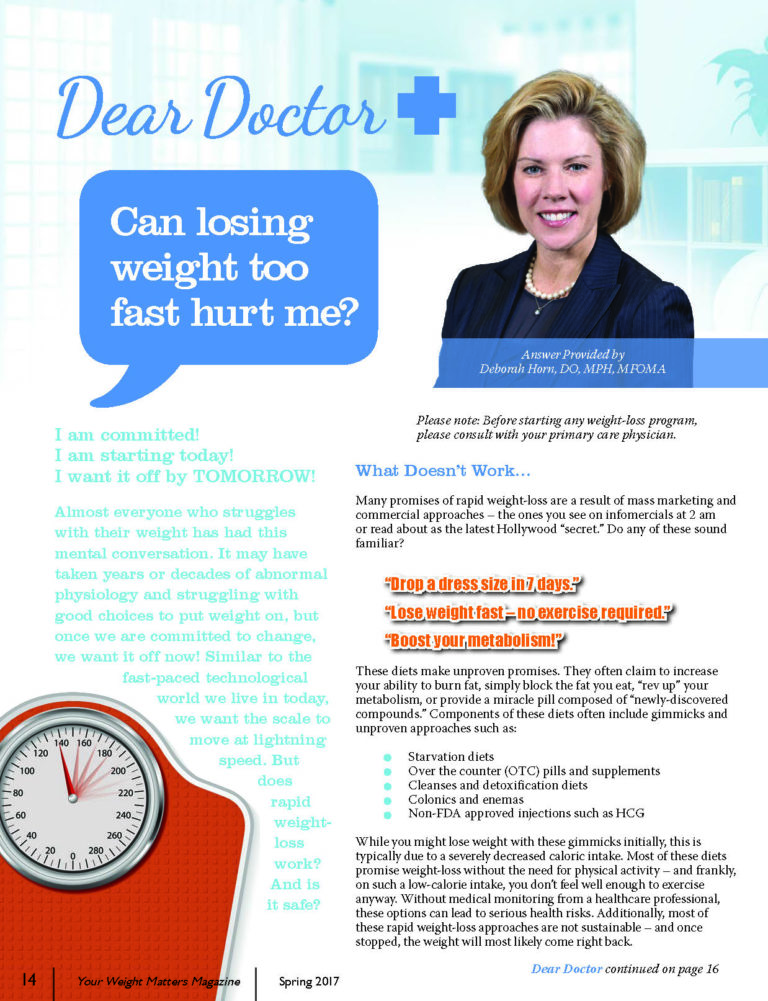
Answer provided by Deborah Horn, DO, MPH, MFOMA
Spring 2017
Please note: Before starting any weight-loss program, please consult with your primary care physician.
I am committed!
I am starting today!
I want it off by TOMORROW!
Almost everyone who struggles with their weight has had this mental conversation. It may have taken years or decades of abnormal physiology and struggling with good choices to put weight on, but once we are committed to change, we want it off now! Similar to the fast-paced technological world we live in today, we want the scale to move at lightning speed. But does rapid weight-loss work? And is it safe?
What Doesn’t Work…
Many promises of rapid weight-loss are a result of mass marketing and commercial approaches – the ones you see on infomercials at 2 am or read about as the latest Hollywood “secret.” Do any of these sound familiar?
“Drop a dress size in 7 days.”
“Lose weight fast – no exercise required.”
“Boost your metabolism!”
These diets make unproven promises. They often claim to increase your ability to burn fat, simply block the fat you eat, “rev up” your metabolism, or provide a miracle pill composed of “newly-discovered compounds.” Components of these diets often include gimmicks and unproven approaches such as:
- Starvation diets
- Over the counter (OTC) pills and supplements
- Cleanses and detoxification diets
- Colonics and enemas
- Non-FDA approved injections such as HCG
While you might lose weight with these gimmicks initially, this is typically due to a severely decreased caloric intake. Most of these diets promise weight-loss without the need for physical activity – and frankly, on such a low-calorie intake, you don’t feel well enough to exercise anyway. Without medical monitoring from a healthcare professional, these options can lead to serious health risks. Additionally, most of these rapid weight-loss approaches are not sustainable – and once stopped, the weight will most likely come right back.
What DOES Work…
There are two medically monitored and proven options for rapid weight-loss:
- Very low calorie diets, “VLCD’s”
- Bariatric surgery
Both of these options are very different from the gimmicks on page 14 in that they have proven results, known side effects, and they allow you to work alongside your healthcare provider to optimize your response.
Option 1: VLCD’s
Medically-monitored VLCD’s are typically diets of less than 800 calories. The plan is often built around a nutritionally complete protein-based meal replacement in the form of a shake, although it can be done with regular food as well. This rapid weight-loss approach focuses on high intake of protein and decreased intake of carbohydrates. Whether protein is built into a shake or taken separately, these diets require an adequate intake of vitamins, minerals, electrolytes and fatty acids. VLCD’s have been shown to demonstrate not just faster weight-loss, but also greater weight-loss at one year than dietary interventions which did not include a VLCD component.
Option 2: Bariatric Surgery
Bariatric surgery can include gastric bypass, gastric sleeve and the gastric band. There are also intermediary procedures available such as the gastric balloon. All of these are currently FDA-approved and create rapid weight-loss in most patients. The rate and total amount of weight-loss can vary widely from person to person.
So, there are some proven and some unproven options for rapid weight-loss. Let’s come back to our initial question. Can losing weight too fast hurt me?
Yes. There are potential negative effects of rapid weight-loss. For this reason and many others, it is recommended that you team up with an obesity medicine specialist, a bariatric surgeon or other experienced healthcare provider with expertise in the treatment of overweight and obesity. Together, you can reduce the risks and optimize the benefits if you choose a rapid weight-loss strategy.
Most Common Rapid Weight-loss Risks:
- Hypoglycemia – This is better known as low blood sugar. If you have diabetes and you are on diabetes medication, your dose of medication can quickly become too high during rapid weight-loss.
What can you do?
Medications like insulin and a group of medications called oral sulfonylureas are particularly important to follow under medical supervision. Diabetes medications often need to be decreased before starting the intervention – or at a minimum, quickly decreased in the very beginning and throughout your weight-loss journey.
- Gallstones – The risk of gallstone formation and acute gallbladder disease requiring gallbladder removal is greater with rapid weight-loss. New gallstones were found in 25-35 percent of individuals on a rapid weight-loss plan. This risk was highest when the rate of weight-loss exceeded approximately 1.5 percent of body weight per week. For example, in a 300-pound individual, this risk would be increased when more than 4.5 pounds per week are lost. Symptoms include right upper abdominal pain – particularly after a meal.
What can you do?
Discuss this with your doctor. If you still have your gallbladder and you have a history of gallstones and/or acute gallbladder disease, you may consider a medication called ursodeoxycholic acid. Studies show that this medication, when used during rapid weight-loss, can decrease gallstone formation from 28-32 percent of individuals to only 2-3 percent of individuals.
- Hypotension – This is better known as low blood pressure. If you are on medication to treat your blood pressure, you can be at risk for dizziness, lightheadedness and potentially falling/injury if your blood pressure becomes too low.
What can you do?
Blood pressure medications often need to be adjusted at the beginning or very early on in a rapid weight-loss plan in order to avoid these risks. Your doctor can help you manage these changes appropriately.
- Muscle Loss – Strong, lean skeletal muscle is one of the major components of metabolism. Muscle is at higher risk of loss during rapid weight-loss attempts when compared to more conservative rates of weight-loss. When we lose weight, individuals typically lose 30-40 percent of their weight from this strong lean muscle. You won’t have any symptoms to identify
the problem.
What can you do?
Make sure you are working with your doctor to monitor your muscle mass as you are losing weight. This is done by frequently measuring your body composition. Getting adequate protein in your diet and stimulating muscles with physical activity may help decrease this loss of lean strong muscle. Scientists are still determining how this may affect your metabolism long-term, and it is likely to be different in different people.
- Dehydration – Decreased fluid intake, decreased salt intake and decreased carbohydrate intake can all lead to decreased total body water. Lightheadedness and/or dizziness are the most common symptoms.
What can you do?
Drink plenty of fluids. If you are on medication for high blood pressure, this may need to be adjusted sooner on a rapid weight-loss plan as some of these medications work by decreasing your total body fluid. With a change in nutrition and weight, you may need to consider a lower dose or the discontinuation of these medications.
- Electrolyte Imbalances – This includes changes in magnesium, calcium, potassium and others. Symptoms can vary.
What can you do?
Any very low-calorie diet or bariatric surgery intervention should include regularly scheduled labs to check these electrolytes and provide supplementation as needed. Your obesity medicine specialist or bariatric surgeon can help you monitor these at appropriate intervals.
A few additional symptoms of rapid weight-loss to watch for include:
- Fatigue – Due to low energy intake
- Headaches – Often caused by dehydration
- Hair loss – Usually transient, but your doctor should check your thyroid levels
- Dizziness – Due to dehydration, low blood pressure, or low blood sugar as described on page 17
- Constipation – Due to dehydration or increased protein in nutritional plan
Rapid weight-loss is just like other health decisions we try to make. It is a matter of weighing the risks versus the benefits. If you and your doctor decide together that you can manage a VLCD or surgical intervention, and that you can maintain follow-up with your healthcare provider, these options are tolerable and the adverse side effects can usually be managed appropriately.
Here are some key points to remember as you consider all of your options:
- Have a Plan – You need a plan to transition off the rapid weight-loss intervention as you approach your goals. This long-term plan needs to be sustainable for you and your lifestyle.
- Consider Medication – There are FDA-approved anti-obesity medications which can help with the rate of weight-loss by controlling hunger and satiety, regardless of whether you choose a moderate rate or rapid rate plan. Evidence is mounting that these anti-obesity medications are just as important during weight maintenance as they are in active weight-loss. Anti-obesity medications do work, so use them!
- Obesity is a Chronic Disease – This is the most important concept – no matter how you choose to approach the disease. While treating any disease brings risk, obesity itself is associated with 236 other diseases – that is real risk.
It’s not your fault – it’s your physiology. Chronic disease requires chronic management and this is where it does become YOUR responsibility to seek care and partner with your doctor to manage your health. Together, you can plan for active phase and maintenance phase treatments that are individualized to you and optimize the benefit versus risk ratio. With many pathways to achieve your goals, the most important thing is to start the conversation today!
About the Author:
Deborah Horn, DO, MPH, MFOMA, is the President of the Obesity Medicine Association and Clinical Assistant Professor in the Department of Surgery at The University of Texas McGovern Medical School at Houston. She is the Medical Director for the UTHealth Center for Obesity Medicine and Metabolic Performance. Dr. Horn was also the recipient of the OAC’s Healthcare Provider Advocate of the Year award, an award given to a healthcare provider who is a tireless advocate for patients, the OAC and the cause of obesity.
Post-operative addiction is often overly simplified as transfer addiction or cross-addiction, assuming individuals “trade” compulsive eating for…
View VideoIt can be challenging to find the right help for your child who has obesity. The first…
View VideoConsidering a robotic surgery procedure? In this Health Talk, you’ll hear from bariatric surgeon Walter Medlin, MD,…
View Video