W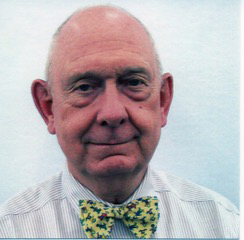 ith September being National Childhood Obesity Awareness Month, we wanted to sit down with an OAC Member who is not just a talented weight management physician, but is also a passionate advocate for children and families navigating childhood obesity.
ith September being National Childhood Obesity Awareness Month, we wanted to sit down with an OAC Member who is not just a talented weight management physician, but is also a passionate advocate for children and families navigating childhood obesity.
Allen Browne, MD, FACS, FAAP, ABOM, spends his career writing, talking, and presenting about childhood obesity. He’s involved with the American Academy of Pediatrics and is on the Pediatric Committees of the Obesity Medicine Association (OMA), The Obesity Society (TOS), and the American Society of Metabolic and Bariatric Surgery (ASMBS). He teaches others about childhood obesity at educational institutions and at local, national, and international meetings. Dr. Browne’s advocacy work also includes fighting to pass the Treat and Reduce Obesity Act (TROA) and for the legislation to include children.
How did you discover the OAC? What drew you to get involved?
I discovered the OAC around 2006 and started to donate money each year. At the time, I was involved in a pediatric weight management program and was getting to know the kids and their families. This experience convinced me that obesity was not their fault and that we did not know the cause of obesity for each child.
Recently, I’ve come to appreciate how important it is to recognize and understand weight bias and stigma when trying to help children with obesity and their families. One of the OAC’s core focuses is weight bias, and for good reason. I decided to help the OAC with education about childhood obesity and how to involve families in reducing bias and stigma. Parents and children need to understand that obesity is not their fault. We must empower them to seek and demand science-based treatment.
How do you approach the sensitivity that is involved with navigating weight in children?
First, appreciate that it’s a sensitive topic. The child and parent have likely experienced many versions of bias and stigma from society. To some degree, many parents and children have internalized this bias and believe it themselves.
The facility in which the child and family seek care has to treat them with respect and dignity. This starts with the staff who greets them, the furniture in the waiting room, the literature in the waiting room, and the pictures in the waiting room. Where and with what attitude they are weighed is important. The exam room equipment and furniture are also important.
More healthcare providers need to be mindful of weight bias and stigma. They need to:
- Convince the family that the obesity is not their fault
- Gain the trust of the child and family
- Treat the child and family with dignity and respect
- Help the child and family understand that there are successful tools to control obesity and improve the child’s present and future health
What can parents and caregivers do to address childhood obesity?
First, realize that treatment and prevention are different. Currently, there are no specific measures a parent can undertake to fully prevent the development of obesity in their child. It depends on genetics and the child’s interaction with their environment. Stress, circadian rhythm, sleep patterns, and environmental chemicals can all influence obesity in varying degrees in some people. Evidence shows that healthy living can improve a child’s health, but it has not been shown to reduce the incidence of obesity. A healthy lifestyle is part of improving health whether the child has obesity or not, and it’s an important part of the treatment for obesity. To successfully treat obesity, the treatment should be interdisciplinary and consider additional science-based tools in combination with healthy living.
How have you seen the childhood obesity landscape change over the years, thanks to the work of advocates and others in the healthcare community? What can we do better at?
The two biggest changes I’ve seen are the appreciation of obesity as a disease and the development of safe, effective treatments.
When I first started working with children with obesity and their families, most had a cultural understanding of obesity. They thought it was caused by eating too much and not exercising enough. It was a “bad habit” and the responsibility of the individual to eat better and move more. Today, we know that obesity is very complex. It has genetic, physiological, and other subconscious factors. It has long-term health consequences, demands long-term care, and can’t be cured by shaming individuals who have it.
Before, the only real treatment we had was metabolic-bariatric surgery. We thought it worked by restricting how much you could eat and by making you unable to absorb enough calories to maintain a higher weight. Then, scientists started to learn that bariatric surgery changes your physiology and the signals sent by your GI tract. Behavioralists, dietitians, and exercise physiologists all began to understand why their efforts weren’t working or had limited results. They couldn’t change a person’s physiology.
No more silos. We all have to work together to treat obesity with a combination of lifestyle management, mental health support, and science-based treatments. We have many tools available to us, and they’re improving every day, as is our understanding of obesity. Together, we must educate ourselves and others, advocate for those affected, and eliminate weight bias and stigma. This needs to involve patients, families, health care providers, health care payers, and policymakers. Access to care is an equity issue and an economic issue.
Finally, we need the public to recognize that obesity is not a person’s fault. It’s not a sign of personal failings. Obesity should be treated with the same level of care and respect as cancer, heart disease, strokes, and other diseases.
Become a Part of the OAC Community
Join the OAC Community today to discover science-based obesity education, find support tools, make meaningful connections and take action to make the world a better place for people living with obesity!
Do You Want to Share Your Story? Whether you have a story about navigating obesity, facing weight stigma, or inspiring others, your voice is important. Visit the OAC’s story project at WeightoftheWorld.com to share yours today. Not sure what to say? Consider one of our question prompts to guide you. If you would like your story to be featured in a future issue of Weight Matters Magazine, please email membership@obesityaction.org.
