Bariatric surgery is a safe and effective treatment option for people with severe obesity and for some with obesity-related health complications. These procedures are recognized for the metabolic and hormonal changes they cause that play a role in hunger (wanting to eat) and satiety (feeling full).
Bariatric surgery is a recognized and accepted approach for both weight loss and treatment of many of the conditions related to obesity. However, not everyone qualifies for bariatric surgery. There are certain requirements people must meet in order to be a candidate for bariatric surgery. In addition to bariatric surgery, FDA-approved bariatric devices are available for the treatment of obesity.
Could You Be a Candidate for Bariatric Surgery?
In 2022, the American Society for Metabolic and Bariatric Surgery (ASMBS) and the International Federation for the Surgery of Obesity and Metabolic Disease (IFSO) issued a joint statement declaring bariatric surgery an effective approach for consistent, long-term weight loss for people with severe obesity. These organizations also established the following criteria for candidacy for bariatric surgery:
- Metabolic and bariatric surgery (MBS) is recommended for individuals with a BMI greater than 35 kg/m2, regardless of the presence, absence, or severity of co-morbidities.
- MBS should be considered for individuals with metabolic disease and a BMI between 30 to 34.9 kg/m2.
- BMI thresholds should be adjusted in the Asian population such that a BMI greater than 25kg/m2 suggests clinical obesity and individuals with a BMI greater than 27.5 kg/m2 should be offered MBS.
- Appropriately selected children/adolescents should be considered for MBS.
Benefits:
Within two to three years following bariatric surgery, patients usually lose 10-35% of their total (pre-surgery) body weight. Results depend on the procedure and vary by individual. If you are considering bariatric surgery, talk with your bariatric surgeon about what your personal expectations for weight loss should be.
Bariatric surgery can help treat obesity-related conditions such as type 2 diabetes, high blood pressure, sleep apnea, and others. Quite often, these conditions are reduced in severity or go into remission. Many surgery patients find they need fewer medications following surgery and may be able to discontinue some completely.
Risks:
Research has shown that some patients who have bariatric surgery have unsatisfactory weight loss or regain much of the weight they lost following surgery. Some lifestyle behaviors, like frequently snacking on high-calorie foods or not exercising regularly, can hinder weight loss and lead to weight regain. Surgical complications can also affect weight loss. Additional complications exist for different surgeries and devices and are discussed in the following pages.
Commonly Used Terms for Bariatric Surgery
In this section, you will see terms you may not be familiar with. In this section, you will find a brief description of these terms as they are used when talking about bariatric surgery.
Open, Laparoscopic and Robotic Procedures
Surgeries in this section are described as being performed either open or laparoscopically. Currently, laparoscopic procedures are more common than open procedures. Your surgeon will decide which approach to use and base this decision on several factors, including their own experience as well as your surgical and medical history. Make sure you discuss with your surgeon beforehand what approach they will use and why.
- Open – An open procedure involves a single incision that opens the abdomen, which provides the surgeon access to the abdominal cavity. The incision can vary in length from as little as three inches to as large as six or more inches.
- Laparoscopic – In laparoscopic surgery, a small video camera is inserted into the abdomen through a small incision. This allows the surgeon to conduct and view the procedure on a video monitor. Both the camera and surgical instruments are inserted through small incisions made in the abdominal wall. The number of incisions will vary depending on the surgical procedure and the surgeon’s experience. Some surgical procedures can be performed with a single incision, while other procedures may involve six or more small incisions.
- Robotic – In robotic surgery, a small three-dimensional camera is inserted into the abdominal cavity. Robotic-controlled arms hold a variety of instruments such as scissors, graspers, and staplers. These are introduced into the abdomen through small incisions. The surgeon sits a computer console to the side of the patient and uses specialized instruments to “drive” the robotic arms to perform the surgery.
Metabolic vs. Non-metabolic
Metabolic Operations – The operations in this category help patients lose weight by altering their gastrointestinal (GI) tracts. Examples include vertical sleeve gastrectomy (VSG), Roux-en-Y gastric bypass (RNYGB), and the biliopancreatic diversion with duodenal switch (BPD/DS).
By altering the GI tract, a patient’s physiological response to eating changes. Metabolic surgery alters the secretion of your gut hormones, which greatly reduces feelings of hunger and is helpful when attempting to lose weight. Recent research indicates that bariatric surgery works by making anatomic and metabolic changes that affect weight loss.
Numerous studies have examined pre-operative and post-operative gut hormone levels after bariatric surgery. A brief summary of hormonal changes after each bariatric procedure is provided in the next sections. Some of these hormones are:
- Ghrelin: Stimulates appetite, increases food storage, and promotes fat storage
- Glucagon-like peptide 1 (GLP-1): Increases satiety (fullness) and reduces stomach emptying
- Peptide YY (PYY): Reduces appetite and increases the efficiency of digestion and nutrient absorption
Non-metabolic Operations – The options in this category provide significant weight loss without altering the gastrointestinal (GI) tract and changing the physiological response to fat loss. One example is the laparoscopic adjustable gastric band (LapBand®). With bandings and with dieting, orexigenic hormones (appetite stimulants) increase, and anorexigenic hormones (appetite suppressants) decrease.
Bariatric Surgery Options
It is no small task to choose a bariatric surgery procedure. There are many choices, various costs, associated risks, and many benefits. It is our goal to provide you with background information on the different types of bariatric surgeries and devices so that you can talk to your healthcare provider about choosing the approach that is best for you.
Bariatric surgery requires proper follow-up and participation in an integrated program that stresses lifestyle modifications (dietary, behavioral, and exercise changes). This will improve the chances for a bariatric surgery patient to maximize their weight loss and maintain it for a lifetime.
Bariatric Surgical Procedures Include:
- Sleeve Gastrectomy
- Roux-en Y Gastric Bypass (RYGB)
- Biliopancreatic Diversion with Duodenal Switch (BPD/DS)
- Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S)
- Adjustable Gastric Banding (LAP-BAND®)
- Robotic Surgery
Please be sure to discuss the various surgical options with your physician to determine which procedure is best for you.
Sleeve Gastrectomy (Metabolic)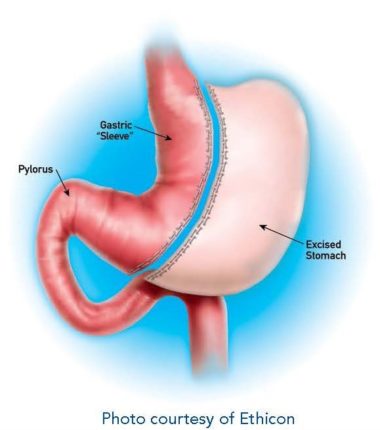
What is a Sleeve Gastrectomy? The vertical sleeve gastrectomy (VSG) is one of the most commonly performed bariatric surgical procedures in America.
It is performed both in hospitals as well as stand-alone ambulatory surgery centers. It is typically performed laparoscopically or robotically. Open VSGs are rare.
How is the Sleeve Gastrectomy Performed? The majority of VSGs are performed laparoscopically. During the VSG, about 75% of the stomach is removed. This leaves a narrow gastric tube, or “sleeve.” No intestines are removed or bypassed during this procedure, and it generally takes about one to two hours to complete. When compared to other bariatric procedures, the VSG can offer a shorter operative time, which can be advantageous for patients with severe heart or lung disease.
Weight-loss: The VSG procedure greatly reduces the size of the stomach and limits the amount of food that can be eaten at one time. It neither decreases the absorption of nutrients nor bypasses the intestines.
After this surgery, patients feel full after eating very small amounts of food. The VSG may also cause a decrease in appetite. On average, by year three, sleeve patients lost approximately 21% of their total body weight from the time of the procedure. In a person who weighs 350 pounds, this is a 74-pound weight loss.
Metabolic/Hormonal Changes: In addition to reducing the size of the stomach, the VSG reduces the amount of ghrelin, a “hunger hormone,” produced by the stomach. The duration of this effect is not clear yet, but most patients have significantly less hunger after the operation. Other hormones in the gastrointestinal (GI) tract may be affected by the sleeve, such as GLP-1 and PYY. Changes to these hormones during a VSG may also decrease appetite.
Complications: The VSG has been used successfully for many individuals affected by severe obesity. The risk of death from a VSG is 0.05% (5 in 10,000) within 90 days after surgery. The risk of major postoperative complications after a VSG is less than 5%, which is typically less than the risk associated with gastric bypass and other metabolic procedures. This is primarily because the small intestine is not divided and reconnected during the VSG.
Complications that can occur within the first month after a VSG include:
-
- A leak from the sleeve, which can cause an infection or abscess
- Deep venous thrombosis (blood clot) or pulmonary embolism
- Narrowing of the sleeve (stricture) requiring endoscopic dilation
- Bleeding
Major complications requiring re-operation are uncommon after recovery from a sleeve gastrectomy and occur in less than 5% of patients. The two most common reasons for re-operative surgery after sleeve gastrectomy are weight regain and severe acid reflux that is not responsive to medical therapy.
Conclusion: The VSG is a common bariatric surgery procedure that can lead to significant weight loss. As with any bariatric surgery procedure, the best results are achieved when the surgery is combined with a multi-disciplinary program that focuses on lifestyle and behavioral changes.
Roux-en-Y Gastric Bypass (Metabolic)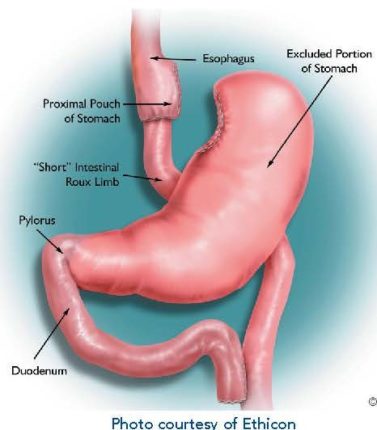
What is a Roux-en-Y Gastric Bypass? The Roux-en-Y Gastric Bypass (RYGB) has been performed since the late 1960s as a treatment for people affected by severe obesity. The operation leads to weight loss through two ways:
-
- A small stomach pouch reduces the amount you can eat.
- A small amount of intestine is bypassed, leading to hormone changes that make you feel less hungry.
How is it Performed? A gastric bypass can be performed open (rare), laparoscopically, or robotically. Operations are typically performed at an inpatient hospital. No matter how the operation is done, the “inside part” is the same.
The surgery involves three basic steps:
-
- Dividing the stomach into two small separate stomachs, creating a small pouch (proximal pouch of stomach) and a larger, excluded lower pouch (remnant pouch of stomach)
- Bypassing part of the small intestine to create the “Short” Intestinal Roux Limb
- Attaching the bypassed intestine (Roux-Limb) to the proximal pouch
How Does It Work? To understand how a gastric bypass leads to weight loss, it is helpful to review how the digestive system works.
When we swallow food, it goes down the esophagus and into the stomach. The stomach can hold huge amounts of food (think about a hot dog eating contest). The stomach then churns the food and mixes it with digestive juices to break the solid food down into a liquid form. That liquid food then leaves the stomach and goes into the small intestine where its nutrients can be absorbed and used as fuel. The small gastric pouch created during the gastric bypass limits the amount of food a person can eat during a meal. The pouch will initially hold a very small amount of food (about half a shot glass full or one tablespoon). However, one-year post-surgery, a gastric bypass patient will be able to eat a meal equal in size to what a seven or eight-year-old child typically eats.
Although the meals after gastric bypass surgery are much smaller than what they were before surgery, they still give the individual the same feeling of fullness they used to get with a much larger meal. Until food is broken down into liquid form, it cannot be absorbed by the small intestine. After a gastric bypass, the food does not turn into liquid until it leaves the “Short Intestinal Roux Limb.” The “Short Intestinal Roux Limb,” therefore, does not absorb all the nutrients from food. This is called malabsorption. This also means vitamins and minerals aren’t absorbed as effectively, so gastric bypass patients must take vitamin and mineral supplements for the remainder of their lives.
The “Short Intestinal Roux Limb” does not handle sugar or starches well, so gastric bypass patients must limit their intake of sugary and starchy foods. If they don’t, they may experience something referred to as dumping syndrome.
Usually, 10-15 minutes after eating sugary or starchy food, the individual who is “dumping” begins to experience many of the following symptoms:
-
- Sweating
- Flushing skin
- Rapid heart rate
- Dizziness
- Low blood pressure
- Abdominal pain
- Vomiting
- Diarrhea
- Shakiness
- Fainting
Dumping can last for 30-45 minutes before going away. Limiting sugars and starches will limit dumping. For many people who have had a gastric bypass, dumping, or the fear of dumping, helps them make better food choices.
Weight-loss: On average, by year one, gastric bypass patients lost approximately 34% of their total body weight (weight at the time of procedure). In a person who weighs 350 pounds, this is a 119-pound weight loss. By year three, bypass patients lost approximately 31.5% of their total body weight.
Metabolic/Hormonal Changes: In addition to reducing the size of the stomach, the gastric bypass reduces the amount of ghrelin, a “hunger hormone” produced by the stomach. The duration of this effect is not clear yet, but most patients have significantly less hunger after the operation. Other GI hormones are affected by the anatomical changes created by the bypass, too. The most important is an increase in a hormone called GLP-1. This hormone is responsible for both creating a sense of fullness and decreasing blood sugar levels.
Complications: The major complications with gastric bypass include bleeding, leaks, infections, bowel blockages, blood clots in the lungs (pulmonary emboli), and death. The chance of dying in the first 90 days after a gastric bypass is less than one in 1,000 people.
Long-term complications that can occur after a gastric bypass include strictures, ulcers, hernias, weight regain, vitamin and mineral deficiencies, and malnutrition. Most of the long-term problems linked to the gastric bypass operation can be prevented by follow-up appointments with your healthcare team.
Conclusion: The gastric bypass is a common bariatric surgery that can lead to significant and sustained weight loss by reducing food intake and altering GI hormones. While there are short-term and long-term risks associated with gastric bypass, many of them can be prevented. As with any weight-loss operation, the best results are achieved when surgery is combined with a program that also focuses on lifestyle and behavioral changes.
Biliopancreatic Diversion with Duodenal Switch (Metabolic)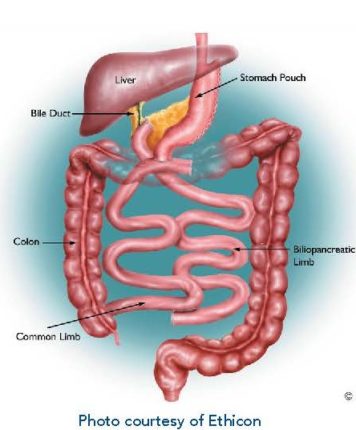
What is a Biliopancreatic Diversion with Duodenal Switch? The Biliopancreatic Diversion with Duodenal Switch (BPD/DS) is an intestinal bypass procedure that can be performed laparoscopically or robotically. It is performed at specialized centers and is not as commonly performed as the gastric bypass or gastric sleeve.
How is it Performed? The outer part of the stomach is removed (approximately two-thirds, like a sleeve gastrectomy) and the intestines are rearranged to shorten the area where food mixes with digestive juices. A portion of the stomach is left with the pylorus still attached and the duodenum beginning at its end. The duodenum is then divided, allowing for the pancreatic and bile drainage to be bypassed. It is a pyloric-saving procedure that eliminates the “dumping” syndrome inherent to the gastric bypass.
Weight-loss: This procedure results in decreased absorption of fat, calories, and other nutrients which may result in increased weight-loss. Foods high in fat are not easily absorbed and will be eliminated, along with their associated high calories. On average, by year three, BPD/DS patients lost approximately 35% of their total body weight (weight at the time of procedure). In a person who weighs 350 pounds, this is a 123-pound weight loss.
As with all bariatric surgery procedures, carbohydrates, and sugars are still absorbed, so eating foods high in sugar and calories can make weight loss difficult or cause weight gain. It is important to remember that eating healthy foods that are low in fat and calories will help with weight loss. The BPD/DS allows patients to increase portion sizes over time and choose a greater variety of foods at each meal.
Metabolic/Hormonal Changes: The metabolic changes that occur with the BPD/DS help patients lose weight and improve their health. The alimentary limb absorbs proteins and sugars from ingested food, but also secretes the GLP-1 hormone in the presence of undigested food. The BPD/DS rearranges this portion of the intestine, causing food to be introduced into the alimentary limb earlier. This enhances GLP-1 secretion, which reduces appetite and releases insulin.
-
- Decrease in Ghrelin = Decrease in hunger
- Increase in PYY = Increase in satiety
- Increase in GLP-1 = Increase in satiety
Complications: Vitamin B-12 deficiencies are not created by the BPD/DS. However, all patients are monitored for iron and B-12 deficiencies, as well as other fat-soluble vitamin deficiencies. BPD/DS patients are specifically monitored for fat-soluble vitamin deficiencies (A, D, E, K) along with zinc. Patients who undergo a BPD/DS can enjoy nutritious foods and eat without the restriction of a small pouch (like with a gastric bypass). The BPD/DS is a more invasive operation compared to the gastric sleeve and gastric bypass. It has a mortality rate of 0.1% (about one in 1,000) within 90 days after surgery.
Conclusion: BPD/DS is a bariatric surgery performed at specialized centers. Its popularity is waning due to the rise of its sister operation, the SADI-S (see the following section). It can lead to significant and sustained weight loss by reducing food intake and altering GI hormones. While there are short and long-term risks associated with BPD/DS, many of these issues can be prevented. As with any weight-loss operation, the best results are achieved when surgery is combined with a program that also focuses on lifestyle and behavioral changes.
Single Anastomosis Duodeno-Ileal Bypass with Sleeve Gastrectomy (SADI-S)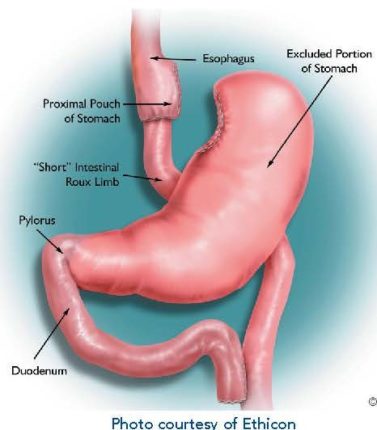
What is SADI-s? The SADI-S procedure is a modification of the BPD/DS operation.
How is it Performed? In most bypass surgeries, surgeons will divide the stomach into an upper and lower part. With SADI-S, they do not divide the stomach into upper and lower parts, but they create a narrow sleeve-shaped stomach by removing the outer “greater curvature” part, including the distinctive fundus (see illustration). Food still goes through the pylorus into the first inch or so of the duodenum. The DS (Duodenal Switch) operations all divide the duodenum very close below the pylorus and connect into the lower part of the small bowel, creating a Duodeno-ileostomy, or Duodeno-Ileal anastomosis. Unlike the BPD/DS where there are two intestinal connections, there is only one “loop” anastomosis in the SADI-S operation.
Weight-loss: The shorter length of “in use” small bowel, compared to the gastric bypass, significantly increases weight loss, resists weight regain, and controls diabetes.
What Are the Benefits of SADI-S? Ulcers and dumping syndrome are less common with SADI-S than with gastric bypass. SADI-S also avoids the second anastomosis that can cause complications as seen with the original BPD/DS, yet the SADI-S results in similar weight-loss.
Complications: Side effects of the bypass/bowel shortening may include a blockage (small bowel obstruction), either from an internal herniation, scar tissue formation, or intussusception. Significant scarring is much less common in the era of robotic and laparoscopic surgery. Daily diarrhea is a significant source of patient dissatisfaction with this operation. Diarrhea can usually be easily avoided by avoiding specific foods. In certain situations, re-operative surgery is necessary to lengthen the intestinal limbs.
Conclusion: SADI-S is a weight-loss operation that is gaining popularity. It is performed at specialized centers and can lead to significant and sustained weight loss by reducing food intake and altering GI hormones. While there are short and long-term risks associated with SADI-S, many of these issues can be prevented. As with any weight-loss operation, the best results are achieved when the surgery is combined with a program that also focuses on lifestyle and behavioral changes.
Adjustable Gastric Banding (Non-Metabolic)
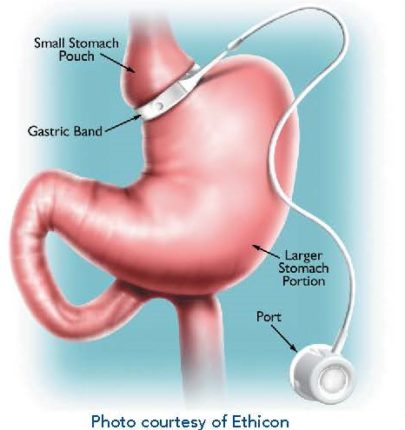
What is Adjustable Gastric Banding? An example of adjustable gastric banding is the LAP-BAND®. This operation involves placing a silicone rubber “belt” around the upper part of the stomach.
How is it Performed? The “belt” essentially separates the stomach into two parts: a tiny upper pouch and a larger lower pouch. The band is connected by tubing to a port (filling reservoir) that sits below the skin of the abdominal wall, usually around the belly button (the port site varies widely by surgeon). The port cannot be seen from the outside, and often cannot be felt. Inside of the “belt” is a balloon that can be filled with fluid through the port. As the balloon fills, it slows the passage of food from the upper pouch to the lower pouch. Patients will feel fuller with smaller amounts of food. You will work with your surgeon to determine the number of band fills or adjustments appropriate for you.
Weight-loss: Weight-loss with an adjustable gastric band is typically slow and steady. Band patients generally lose one to two pounds per week during the first year after band placement. On average, by year one, band patients lose approximately 14% of their total body weight (weight at time of procedure). In a person who weighs 350 pounds, this is a 49-pound weight-loss. By year three, band patients lose approximately 15.9% of their total body weight.
Metabolic/Hormonal Changes: There are minimal metabolic and hormonal changes with this procedure.
What Are the Benefits of Gastric Banding? The LAP-BAND® is FDA-approved for patients with a BMI of 40 or greater, or with a BMI of at least 30 with one or more obesity-related conditions.
There are several other features that make the adjustable gastric band appealing:
-
- There is minimal stress to the body at the time of surgery because the band is almost always placed laparoscopically and does not involve cutting the stomach or rerouting to the intestines.
- Most patients can go home the same day or the next morning.
- Recover from surgery is usually quick, and most people return to work a week or so after surgery.
- The adjustability of the band makes it unique among weight loss operations. This feature allows the possibility of making band adjustments based on the individual weight loss goals and needs of the patient.
- The stomach and intestines are not bypassed, so vitamin, mineral and nutrition problems after banding are less common. However, many programs still recommend taking vitamin supplements after banding.
- While it is a non-metabolic procedure, some patients have reported reduced hunger.
Complications: Patients contemplating adjustable gastric banding must be comfortable with the thought of having a medical device in them for life. Although the band has an excellent safety profile, some complications can occur with any weight-loss operation, and the band is no different. It is important for patients to have routine follow-up appointments with their healthcare team for adjustments and monitoring. About 30-50% of patients will require a second operation to address a problem with their band.
Potential complications include band slippage or gastric prolapse, band erosion through the stomach, or tubing leakage. The risk of death from band surgery is equal to or less than 0.1% (one in 1000) within 30 days after surgery. However, many centers report even lower rates. The adjustable gastric band can be removed, if necessary.
It is important to understand that the band is not a short-term fix. It is intended to be left in your body indefinitely. As with other medical devices implanted in the body, long-term effects (20 to 30 years) are unknown at this time with the band.
In the first year after surgery, when band adjustments may be required more frequently, patients need to be available for regular follow-ups with their healthcare team. In deciding if banding is right for you, it is important to consider both the time and distance involved in traveling to where the adjustments will be performed. Adjustments are made by filling the band through the port with fluid through a needle. Band patients do not suffer adverse effects from eating sugars (dumping syndrome), so they need to be more disciplined in their food choices. Foods and beverages like sodas, ice cream, cakes, and cookies slide through the band easily. These choices will not lead to the desired goal of significant weight loss.
Conclusion: Adjustable gastric banding is an effective weight-loss operation that can lead to meaningful, long-term weight loss. Still, individuals need to make lifestyle changes and learn to work with the band to be successful.
Robotic Surgery
What is Robotic Surgery? A robot is not an independent thinking machine that performs surgery at the press of a button, like a microwave. Instead, the robot is an accessory that allows the surgeon to better visualize tissue and have near-complete control during the procedure. Movement and precision are vastly increased. To get an idea of how it works, try to use only your thumb and pointer finger to pinch and rotate/twist whatever you pick up for the next hour. Compare that to using your entire hand and wrist with all the intricacies of bending and rotating them as well. That is the biggest difference between laparoscopic and robotic surgeries.
How is it Performed? In bariatric surgery, the procedure is started laparoscopically. Robotic arms are connected while the surgeon sits at a hub and controls all aspects of movement, including cautery and suturing within the abdomen. The operating team is right at the patient’s side, assisting with changing instruments and communicating with the surgeon directly via microphones and speakers. From the surgeon’s standpoint, he/she can sit for the duration of the robotic portion with an amazingly high-definition picture that is rendered in 3-D. The mechanics of the robot allow for the surgeon’s movements to be smoothly mimicked by the instruments inside the abdomen. The robot can use cautery and scissors and allows the surgeon to suture with ease. Put simply, the robot is a great tool for the surgeon. It makes the operation smoother and easier for both the patient and the surgeon while keeping everyone’s safety intact.
Weight-loss: Weight loss is dependent on what type of bariatric surgery you have.
What Are the Risks and Benefits of Robotic Surgery?
Some of the benefits of robotic surgery include:
-
- Better visual view for the surgeon
- Improved efficiency in the work environment and precision/accuracy
- Improved technique with the elimination of a hand tremor
- Surgeons get less fatigued through the procedure and are more capable of performing surgery
- More control for the surgeon
- Equal safety outcomes compared to laparoscopic surgery
- Options for telesurgery
- Less reported pain at incision sites
Some of the risks of robotic surgery include:
-
- More expensive for the hospital (although finance options are available)
- Surgeons go through years of training
- Surgeons can normally feel when something isn’t right, but robots can’t
- Large piece of equipment
- Longer duration of surgery
Conclusion: There are many benefits to participating in robotic surgery. Ultimately, whether you can or should receive robotic surgery depends on your surgeon. If you are interested in having robotic surgery, you should consult with your healthcare provider to see if it is the right choice for you.
Bariatric Devices
Bariatric devices are safe, effective treatment options for individuals with obesity or severe obesity. Currently, there are two bariatric devices approved by the FDA: the ORBERA™Intragastric Balloon and Plenity®.
ORBERA™Intragastric Balloon (Non-Metabolic)
What Are Intragastric Balloons? Intragastric balloons are soft, durable silicone spheres that promote proper portion control by occupying stomach space and promoting fullness, resulting in smaller meals.
Who Qualifies for an Intragastric Balloon? Intragastric balloons are intended for adult patients who have a body mass index (BMI) of 30 to 40. Intragastric balloons are also an option for individuals who do not want or do not qualify for more invasive bariatric surgery.
How Does It Work? The ORBRERA™Intragastric Balloon is a single balloon that is inserted into the stomach using an endoscope. It is then filled with saline (salt water) until it is about the size of a grapefruit. Intragastric balloons occupy some of the existing space in your stomach for six months, serving as built-in portion control. It allows you to feel full and satisfied with less food. After six months, the balloon is removed in the same way it was placed, endoscopically. Through a procedure done under a mild sedative, it is deflated and then removed through the esophagus and mouth.
What Are the Risks? More than 15,000 balloons of the liquid-filled type have been placed in the U.S., and over 350,000 have been placed worldwide. The device has been through extensive trials that show relative safety and effectiveness. However, nothing is absolutely safe and without risks. The FDA is doing its job to follow up on the ongoing use of these devices. The intragastric balloon treatment has a mortality rate of less than one in 10,000 and is considered a safe procedure.
Weight-loss: U.S. clinical trial data on ORBERA™ showed that within six months, the average person lost 3.1 times the amount of weight as compared with diet and exercise alone. In real numbers, that means patients with ORBERA™lost an average of 21.8 pounds (10.2% of their body weight) after the device had been in place for six months. The clinical trial for ORBERA™ also demonstrated that three months after the device was removed (nine months after device placement), ORBERA™ patients maintained an average weight loss of 19.4 pounds. During the trial, those patients who participated in a behavior modification program (diet, exercise, and emotional coaching) but did not receive the ORBERA™ balloon, only lost an average of seven pounds (3.3% of their body weight).
Concerns: Following the procedure, you may experience some discomfort as your stomach gets used to the intragastric balloon. Side effects may include nausea, vomiting, and gastric discomfort during the first week. These normal and expected side effects can be relieved with medication and guidance from your HCP. These side effects are normal and are to be expected.
Plentity®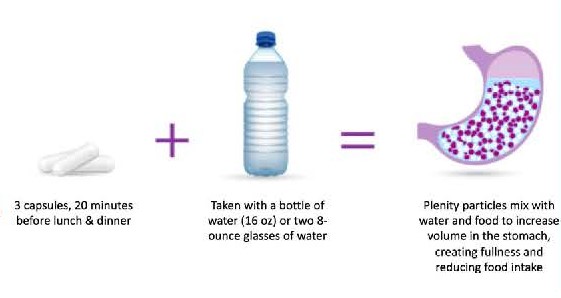
What is Plentity®? Plentity® is a new class of weight loss options called “super absorbent hydrogels.” Technically the Food and Drug Administration (FDA) cleared Plentity® as a device, but it is actually a pill (capsule) that is taken daily with lunch and dinner to help with weight loss. Through some impressive food engineering, these capsules release thousands of particles that swell and enlarge in the stomach. The particles then mix with food and travel through the intestines, where they increase feelings of fullness and help patients lose weight.
Weight-loss: Plentity®, combined with diet and exercise, may help patients lose an average of 5-10% of their total body weight. Some patients may be extra responsive to Plentity® and lose more weight than others, averaging close to 10% weight loss. Those who tend to respond better to Plentity® are those who lose 3% or more of their weight in the first eight weeks of using it. It should also be noted that Plentity® is meant to be used with a proper diet and exercise for the best weight-loss outcomes.
How Does Plentity® Work? The pill is swallowed with meals and contains thousands of small particles that expand up to 100 times when taken with water. It has the firmness of solid food, similar to vegetables. Plentity® mixes with food in the stomach and travels down the intestines in this enlarged form. The pill expands in the stomach and stays expanded as it works its way through the first part of the intestines. When Plentity® reaches the end of the intestines (colon or large intestine), the water is reabsorbed by the intestines. When the intestines reabsorb the water, the particles shrink down to their original small size and get eliminated with the next bowel movement.
Complications: The most common side effects of Plentity® affect the digestive system. These side effects include diarrhea, decreased bowel movements, constipation, abdominal digestion, flatulence (gas), and nausea. This product has not been studied in patients who have already received bariatric surgery.
Conclusion: Plentity® can generally be used safely by anyone who wants to lose weight for various reasons. Plentity® moves through the intestines naturally and the results help patients feel fuller, eat less, and lose weight.

