What to do When You’re Denied (Bariatric) Weight-loss Surgery

by Pam Davis, RN, CBN, MBA
Fall 2011
*Please note: The terms “bariatric” and “weight-loss” are used interchangeably throughout this article.
Kick, scream, yell, cry, curse and take a deep breath. Kick, scream, yell, cry, curse again and take a few more deep breaths. Of one thing you can be sure, you are not the first person to be denied approval for weight-loss surgery by your insurance; nor will you be the last. While access to care has most certainly improved for many in the last few years, coverage for weight-loss surgery is not standardized and can vary tremendously based on your employer and your insurance plan.
Your Coverage Depends on Your Employer
Frequently, we may be quick to blame the insurer for lack of coverage. It is important to make a clarification. In order to provide coverage for their employees, companies must purchase a “rider” for weight-loss (bariatric) surgery coverage. Self-insured employers (typically larger employers where the money paid for their claims comes from their own pocket) frequently provide weight-loss surgery benefits.
In this circumstance, where the company has elected to provide coverage, the insurance company now applies their standard criteria to those seeking surgery. If the employer has coverage and you meet the criteria on the plan, you are approved, right? Well, not always.
It has been my observation throughout the last several years that many times, it appears as if our patients are denied the first time for a multitude of reasons:
“We did not receive the letter from your primary care physician.” – Rest assured, it was sent.
“We do not have documentation of failed previous weight-loss attempts.” – This too was sent.
“Documentation of weight for one of the previous five years is missing.” – Uh-huh, sure it is.
The good news here is if your employer is self-insured with a bariatric surgery benefit and you have documentation, you meet all of the criteria on the plan and you are denied, they do not have a leg to stand on! Ask your surgeon’s office to arrange a “peer-to-peer” review. This is where your surgeon will speak with the medical director at the insurance company to review your documentation and to point out how you meet the criteria.
As an alternative, you may also ask the human resources director at your company to intervene on your behalf. Whatever you do, please, please do not hang your head and say, “Oh, it just wasn’t meant to be” or “God must not have wanted me to have surgery.” Please do not give the insurer that power because they will surely take it. I also encourage you to consider hiring a professional, such as an obesity lawyer, to intervene on your behalf.
If your employer is self-insured but they do not have a bariatric surgery benefit, please visit the OAC Web site. There, you can find a fact sheet titled, “Why it makes sense to provide treatment for obesity through bariatric surgery.” This fact sheet is designed for you to share with your employer, insurance provider, elected officials and others. It provides in-depth information on the benefits of weight-loss surgery. All of that research you’ve done on bariatric surgery? Take it too. Make sure your decision makers are informed. You cannot rely on someone else to educate them for you.
The majority of standard insurance plans sold to businesses do not have bariatric surgery benefits included. For smaller businesses that are not self-insured, they pay a set amount of money per employee to the insurance company; the money goes there and stays there regardless of how much is paid in claims. In most states, these small companies have no access to purchase an insurance plan that provides bariatric surgery coverage. The plan benefit will typically read, “bariatric (weight-loss) surgery is an exclusion on this plan.”
Advocacy is Important in the Fight for Access to Care
The long-term solution is to advocate for access to care. Advocacy can often be intimidating to an individual who has never advocated for a cause; however, the OAC has made advocating to your elected officials for coverage of weight-loss surgery extremely easy. The OAC’s Legislative Action Center is designed to help you advocate to your elected officials (capwiz.com/obesityaction/home). Simply type in your zip code and you’ll instantly have access to all your elected officials’ contact information. For tips on what to write to your elected officials, please click here.
Alternative Ways to Access Care
While you are advocating for future coverage, it may not be enough to help you in your immediate goal to have surgery. In this instance, do your research; locate a Bariatric Surgery Center of Excellence program and surgeon that offer a comprehensive program at a reduced self-pay (cash) rate that includes coverage of complications or readmissions through the BLIS program (www.bliscompany.com). Then approach your employer with the information from your bariatric program, the resources listed at the end of this article, and the total costs to self-pay for surgery (that includes covering any potential complications and ask them to pay the surgeon and program directly or ask them to share the cost with you).
You and your employer will both benefit from you being a healthier and more productive employee and you do not have to go through your insurance company. Additionally, there are healthcare financing companies available for those choosing to self-pay for surgery, bypassing insurance altogether.
To Do List if Denied:
- Speak with your human resources department – is your company self-insured?
- Find out if you meet their criteria.
- Make sure it is documented that you meet their criteria.
- Work with your surgeon/program to complete a peer-to-peer review if your company covers surgery and you meet the criteria.
- Consider hiring an advocate, such as a lawyer that specializes in representing individuals affected by obesity.
- Educate yourself and others using the resources mentioned in this article.
- Gather your documentation, speak with your human resources department or company owner regarding cost sharing a self-pay rate at a comprehensive program with BLIS coverage.
It’s about Education and Advocacy
“Thank you for your interest in bariatric surgery, unfortunately your plan does not cover this procedure.”
“Weight-loss surgery is an excluded benefit from your plan.”
“You have been denied access to weight-loss surgery.”
Unfortunately, these statements are not uncommon in today’s world of navigating one’s insurance policy. Each day, hundreds of individuals are denied access to bariatric surgery. Being denied surgery often leads to feeling lost and hopeless; however, there is still hope and it comes in the form of education and advocacy.
One of the most impactful messages that can be sent to an insurance provider, employer or elected official is a message from someone who was affected by obesity and received weight-loss surgery. Often times, weight-loss surgery patients are an excellent resource for information and support and can speak loudly and positively in regards to the impact of weight-loss surgery on an individual’s quality of health and life.
You can connect with weight-loss surgery patients in a variety of ways, such as attending a post-surgery support group meeting; social networking on Facebook, Twitter, etc; or asking your surgeon if they can help you connect with a post-surgery patient for more information.
As you can see, hearing that you’ve been denied weight-loss surgery does not have to be the “final word.” As an informed citizen, you have many options to first educate yourself on the procedure and then advocate to your insurance provider, employer, elected officials and others for coverage.
About the Author:
Pam Davis, RN, CBN, is a certified bariatric nurse and the Program Director for Centennial Center for the Treatment of Obesity in Nashville, Tenn. Pam is the Vice-chairman of the OAC.
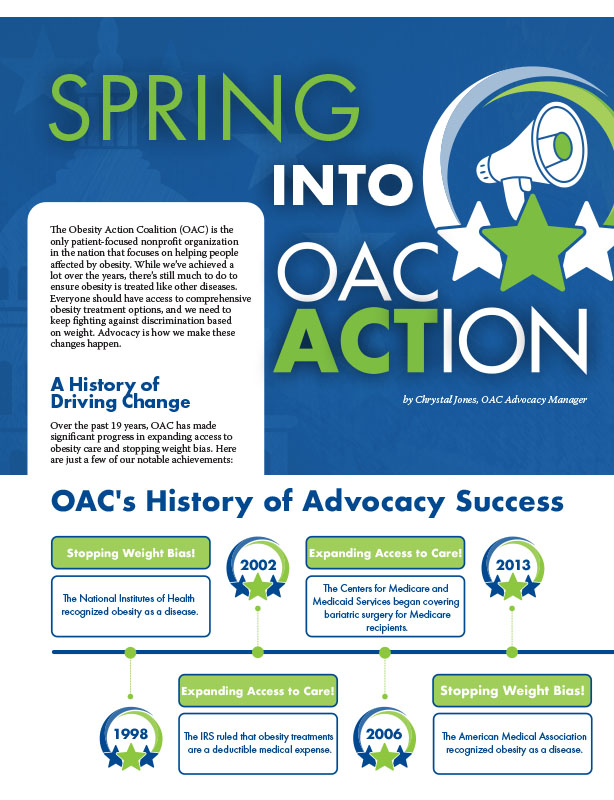
by Chrystal Jones, OAC Advocacy Manager Spring 2024 The Obesity Action Coalition (OAC) is the only patient-focused…
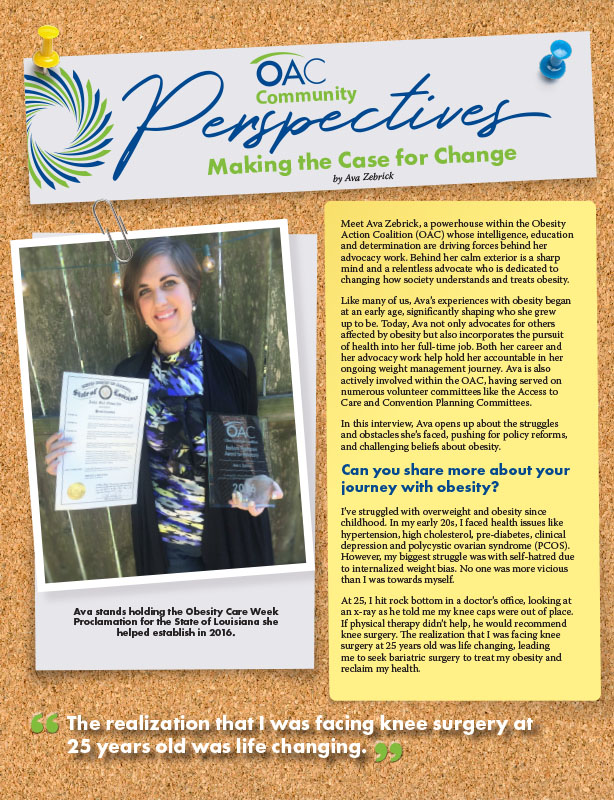
Read Articleby Ava Zebrick Spring 2024 Meet Ava Zebrick, a powerhouse within the Obesity Action Coalition (OAC) whose…
Read ArticleThe OAC is honored to welcome three new members to the OAC National Board of Directors. Jason Krynicki,…
Read Article