Understanding the Childhood Obesity Epidemic


by William Cochran, MD
Fall 2005
“Doctor, is my child overweight?” “Oh no, it is just baby fat and he’ll grow out it.” Does your son or daughter have excess weight or obesity? Is it indeed just baby fat, and will they outgrow it?
Pediatric obesity is now of epidemic proportions in the United States. Pediatric overweight and obesity now affects more than 30 percent of children, making it the most common chronic disease of childhood.
Pediatric obesity is not just a cosmetic problem; it is a real health problem that can be associated with significant issues in childhood and in adulthood. Therefore, parents of overweight young children should not just ignore this issue, but should actively seek out help to determine why their child is overweight and what they can do to help rectify the situation.
Understanding Obesity in Children
When infants are born, they have comparatively more fat; however, this is normal and appropriate. This relatively greater amount of fat provides the infant with some nutritional reserve when they are most vulnerable and adjusting to life outside the womb. This greater amount of fat decreases as the infant grows older and throughout the first several years of life.
Around five years of age, children have the lowest amount of fat and have the lowest body mass index (BMI) – a relationship between weight and height. If a child is getting overweight between two and five years of age, this is not normal and it is not just “baby fat.” Likewise, after five years of age, an overweight child should not be treated as if it is just “baby fat” and told they will outgrow it and not to worry.
In reality, if your child has excess weight or obesity, you do have a cause for worry. The earlier in the child’s life that you make changes a child’s lifestyle in regards to nutrition and physical activity, the easier it is.
Measuring Obesity in Children
You may be confused with the many new terms related to obesity. There is good reason for this confusion as there is controversy over the definitions related to obesity. For adults more than 18 years of age, the definitions are based on BMI. BMI can be calculated using pounds, inches or kilograms and meters using the following formulas:
Using pounds and inches:
BMI = Weight in pounds x 703
(Height in inches) x (Height in inches)
Using kilograms and meters:
BMI = Weight in kilograms
(Height in meters) x (Height in meters)
The normal range of BMI for adults is 18.5-24.9. A BMI of less than 18.5 is considered underweight. A BMI between 25 and 29.9 is considered overweight while a BMI of 30 and over is considered severe obesity. Some also define morbid obesity as a BMI greater than 40.
For children, BMI is calculated in the same fashion as for adults, but there are no absolute numbers of BMI defining normal and overweight. Instead, you have to calculate BMI and plot it on a BMI curve and find the percentile for a child. There is a BMI curve for males and a separate one for females, ages two to 18 years.
The exact definition does not matter as much as knowing what the BMI percentile of the child is and if it is normal or abnormal, increasing or decreasing. For simplicity sake, we will use excess weight and obesity interchangeably.
For children less than two years of age there is no BMI curve available. Instead, you can plot the measurement on the “weight for length curve” that can be found on the “growth curve” used by healthcare providers. Normal weight is when this measurement falls between the five and 95 percentiles. A child with a “weight for length” that plots less than five percent is considered underweight and greater than the 95 percent is considered overweight.
Causes of Childhood Obesity
Changes in the living environment (how we live, eat and act) is the major factor that has contributed to the current problem. There have been several dietary changes that have transpired over the last 20 to 30 years which have contributed to obesity.
One major factor is the frequency with which people eat out. It is now estimated that approximately 40 to 50 percent of every dollar that is spent on food is spent on food outside the home (i.e. restaurants, cafeterias, sporting events, etc.). When people eat out they tend to eat a larger quantity of food (calories) than when they eat at home. Also, foods that are consumed in restaurants tend to have more fat (higher caloric density) which in turn contributes to excessive intake of calories. This also tends to be true for meals purchased in the school cafeteria. Providing children with money to buy their lunch at school also poses another potential problem.
Portion sizes have also increased. This is true for packaged foods and fast food restaurants. Take french fries for example. A portion size is actually 12 french fries. Most fast food restaurants have small or medium french fries, but sell more large or extra-large french fries. People do not think that a large order may actually be two or three portions.
Also, soda sizes have significantly increased. The average serving size of a soda was 6 and a half ounces in 1950, and increased to 12 ounces in the 1960’s and 20 ounces in the 1990’s. Currently, 24 and 32 ounce sodas are marketed, with a 32 ounce soda containing approximately 400 calories. The consumption of soda by children has increased throughout the last 20 years by 300 percent. Fifty to more than 80 percent of children consume at least one soda per day and 20 percent of children consume more than four per day. Scientific studies have documented a 60 percent increase risk of obesity for every regular soda consumed per day.
Box drinks, juice, fruit drinks and sports drinks present another significant problem. These beverages contain a significant amount of calories and it is estimated that 20 percent of children who are currently overweight are overweight due to excessive caloric intake from beverages.
Another major factor in contributing to the pediatric obesity epidemic is the increased sedentary lifestyle of children. School-aged children spend most of their day in school where their only activity comes during recess or physical education classes. In the past, physical education was required on a daily basis. Currently, only eight percent of elementary schools and less than seven percent of middle schools and high schools have daily physical education requirements in the U.S.
Children are also more sedentary outside of school, which is due to increased time spent doing sedentary activities such as watching television, playing video games or using the computer. Only 50 percent of children, 12 to 21 years of age, regularly participate in rigorous physical activity, while 25 percent of children report no physical activity. The average child spends two hours a day watching television, but 26 percent of children watch at least four hours of television per day.
Studies indicate that when children watch more than two hours of television per day there is a significant increased risk of obesity as well as high blood pressure. Studies have also determined that children who eat in front of the television consume higher fat and salt containing foods and less fruits and vegetables than children who do not eat in front of the TV.
Staggering Statistics
- Only eight percent of elementary schools, and less than seven percent of middle schools and high schools, have daily physical education requirements in the U.S.
- Only 50 percent of children, 12 to 21 years of age, regularly participate in rigorous physical activity
- Twenty-five percent of children, 12 to 21 years of age, report no physical activity
- The average child spends two hours a day watching television
- Twenty-six percent of children watch at least four hours of television per day
Correlation Between Childhood Obesity and Adulthood Obesity
Pediatric obesity is a real and very significant health problem that is associated with adverse effects on health in childhood as well as adulthood. There is a high likelihood of a child with obesity becoming an adult with obesity. This risk increases as the child gets older.
The risk that a five year-old child with obesity remains affected by obesity as an adult is approximately 50 percent. This increases to more than 80 percent for an adolescent with obesity. On the other hand, the risk of a normal weight child becoming affected by obesity as an adult is only seven percent.
Childhood obesity also has adverse effects on health during childhood. The most common consequence of childhood obesity is the psychosocial effect. It has been shown that adolescents with obesity have higher rates of poor self esteem, and this negative self image may carry over into adulthood. There may also be increased rates of depression in children who are overweight.
Our society also discriminates against individuals with obesity, females more so than males. It has been documented that females with obesity have lower acceptance rates for college than non-overweight females with the same grades and standardized test scores. The National Longitudinal Survey of Youth study noted that female adolescent with obesity as young adults had less education, less income, higher poverty rate and decreased rate of marriage as compared to non-overweight adolescent females.
Health Risks of Childhood Obesity
There are multiple medical conditions associated with obesity in childhood. The most common include insulin resistance (the first step towards developing diabetes), hypertension, liver problems and hyperlipidemia (elevated cholesterol and/or triglyceride). While these typically do not cause many problems in childhood, some children will develop diabetes or severe liver disease, including cirrhosis. Other problems that can occur include joint problems, menstrual problems, gallbladder disease, sleep apnea and headaches.
Treating Childhood Obesity
Treatment of pediatric obesity is a family affair and needs to be directed at the family, not just the child. This is extremely important since the home environment and family support are important factors when trying to address pediatric obesity. If the child is the only one making changes in their life, they are less likely to be successful and are then made to feel different. Likewise, parents who do not make healthier changes in their lives are likely to undermine the child’s attempts.
Prior to addressing the treatment of childhood obesity, you must first assess the readiness of the child and the family to make changes. If the child is very depressed, this needs to be addressed prior to working on the child’s weight problem. If a depressed child attempts weight-loss and is unsuccessful, this may worsen their depression or lower their self-esteem.
Similarly, if there is a lot of stress in the family at that time it is not ideal to try and tackle yet another major issue. In some situations where there is significant depression or stress, it may be most appropriate for the child and the family to seek counseling to address these issues. In addition, if parents express little concern regarding their child being overweight, they are not ready to make the necessary changes.
Treatment of pediatric obesity is not accomplished by just dieting. You need to address multiple aspects of the child’s and the family’s lifestyle, nutrition and physical activity patterns. Prior to discussing any treatment plans, you first must determine what the desired goals are. If your child is overweight, or at risk for becoming overweight, it is important to work with your healthcare provider to develop an individualized plan of care that includes realistic goals and action steps.
Treatment Goals
The goals of treatment of pediatric obesity can be divided into three major areas: behavioral goals, medical goals and weight goals. The behavioral goals are to promote lifelong healthy eating and activity behaviors. Medical goals are to prevent complications of obesity in childhood and potentially adulthood, as well as improve or resolve existing complications of obesity. The weight goals are dependent on the child’s age and the presence or absence of associated co-morbidities.
Taking the First Steps
The first step for all overweight children is to establish weight maintenance. For children two to seven years of age with a BMI between 85-95 percent, weight maintenance is the primary goal. This is because the child will be growing taller and they have the time as well as the ability to “grow into their weight.” For those with a BMI greater than 95 percent and no associated complications, weight maintenance is still the overall goal. For those whose BMI is greater than 95 percent and have an associated co-morbidity, weight-loss should be strived for after weight maintenance is achieved. Children seven to 18 years of age with a BMI between 85-95 percent and who have no complications, weight maintenance is reasonable. However, close follow-up is needed to ensure that they are not becoming more overweight or develop a complication of obesity.
For those who have an associated co-morbidity and/or whose BMI is greater than 95 percent, weight-loss should be strived for after weight maintenance is achieved. When weight-loss is desired, it needs to be stressed that gradual weight-loss is preferable to rapid weight-loss. It is better to make gradual changes that can be maintained over time, resulting in gradual weight-loss. Ideally, you should not try to lose more than one to two pounds per week.
Parents and Treating Childhood Obesity
Parents are of vital importance in the treatment of pediatric obesity. Parents act as role models for their children regarding nutrition and physical activity. It is extremely important for an overweight child to see the parents being an example of what they want their child to do. Treatment needs to be family-based and individualized. By obtaining a good dietary, physical and lifestyle history, areas of potential concern for that child and family can be identified and then addressed.
Here are tips to help change a family’s lifestyle, nutrition habits and activity level:
Lifestyle
Eat as a family.
Slow down the eating process.
Have special family time that is physically active.
Limit eating out or getting take-out food.
Pack lunch for school instead of buying lunch.
Do not have a television in the child’s bedroom.
Limit computer time to a maximum of 1-2 hours per day.
Do not eat in front of the television.
Do not use food as a reward.
Nutrition
Eat healthy, well balanced meals and snacks.
Plan meals and snacks in advance.
Offer the child a choice of healthy foods to eat.
Limit intake of calories from beverages.
Eat appropriate portion size for the child’s age.
Limit calorically dense foods (i.e. high fat, high sugary foods).
Limit treats, but do not eliminate them.
Physical Activity
Encourage daily physical activity.
Have a variety of physical activities that can be done.
Be physically active with others.
Limit sedentary activity.
Three Major Areas of Treatment
Treatment of pediatric obesity needs to focus on three major areas: lifestyle, nutrition and physical activity. As you approach the treatment of obesity, it is important this is done in a gradual and stepwise fashion. Once some problem areas are identified, you may consider discussing a few of them and then ask the child to pick one to work on at that time. If you present a long list of things that the child and family need to change, they may feel overwhelmed and are likely to not make any attempt.
In addition, once one or two issues are agreed upon, close follow-up is required to monitor changes, as well as to give positive reinforcement for change in behavior even if no weight is lost. The greater the period of time between appointments with the primary care provider the less likely they are to be successful. Once the initial behavior change has been successfully accomplished, the child and family should move on to the next desired change, but at the same time continue to monitor the initial change.
Medicationsand Childhood Obesity
There are a number of medications both over-the-counter and prescription that are available for the treatment of obesity. These are not frequently used in the initial phase of treatment of pediatric obesity; however, the primary treatment modality is behavior modification and lifestyle changes. Some children with significant obesity, especially those associated with other co-morbidities, may benefit from pharmacologic therapy as well. This should be done only under the direction of a physician knowledgeable in the area of pediatric obesity
Surgery and Treating Childhood Obesity
Bariatric surgery (weight-loss surgery) for adults with severe obesity is now being done with increased frequency. This surgery is safe and effective, but is to be used only for those with morbid obesity who meet specific criteria. At this time bariatric surgery should be considered investigational and should only be done in institutions with a comprehensive pediatric weight management program and by surgeons experienced with this type of surgery in children.
About the Author:
Lisa Saff Koche, MD, is the Medical Director for Spectra Healthcare and an Associate Clinical Professor at the University of South Florida in Tampa. Dr. Koche has practiced in obesity for seven years with aggressive medical management as well as complete medical support for bariatric surgery patients.
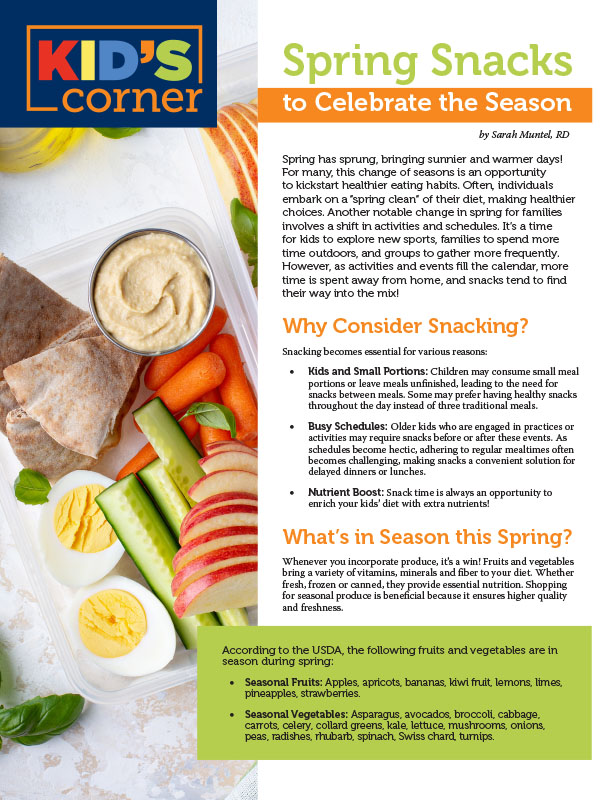
by Sarah Muntel, RD Spring 2024 Spring has sprung, bringing sunnier and warmer days! For many, this…
Read Articleby Yelena Kibasova Spring 2024 The fitness world is evolving, with new trends and innovations that promise…
Read Articleby Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read Article