The Gas You Pass Following Bariatric Surgery: What’s behind this Post-op Issue

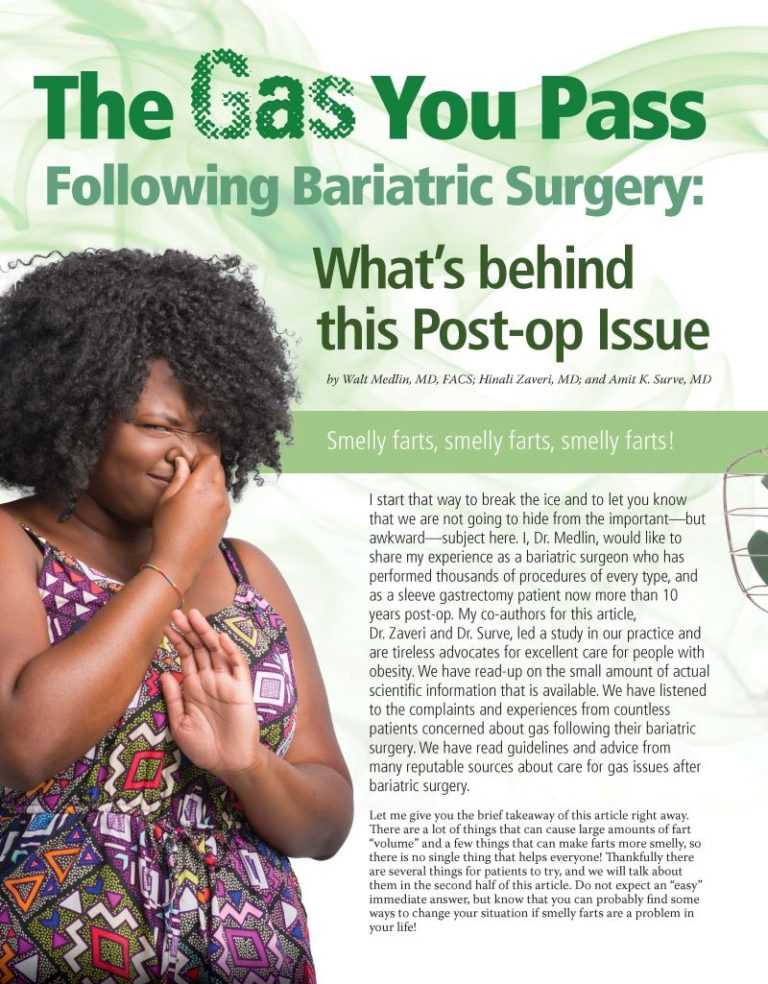
by Walt Medlin, MD, FACS; Hinali Zaveri, MD; and Amit K. Surve, MD
Spring 2019
Smelly farts, smelly farts, smelly farts!
I start that way to break the ice and to let you know that we are not going to hide from the important—but awkward—subject here. I, Dr. Medlin, would like to share my experience as a bariatric surgeon who has performed thousands of procedures of every type, and as a sleeve gastrectomy patient now more than 10 years post-op. My co-authors for this article,Dr. Zaveri and Dr. Surve, led a study in our practice and are tireless advocates for excellent care for people with obesity. We have read-up on the small amount of actual scientific information that is available. We have listened to the complaints and experiences from countless patients concerned about gas following their bariatric surgery. We have read guidelines and advice from many reputable sources about care for gas issues after bariatric surgery.
Let me give you the brief takeaway of this article right away. There are a lot of things that can cause large amounts of fart “volume” and a few things that can make farts more smelly, so there is no single thing that helps everyone! Thankfully there are several things for patients to try, and we will talk about them in the second half of this article. Do not expect an “easy” immediate answer, but know that you can probably find some ways to change your situation if smelly farts are a problem in your life!
Living with Gas after Surgery
On the serious side, being smelly can really make life miserable—especially at work or during times where we are trapped in small places with others. For example, elevators can be intimidating to people who can’t predict when their worst moments are coming. Airplanes and group offices can also be unbearable.
Here is a quick personal story about my own post-op experience:
When I was in my first year or two after having my sleeve gastrectomy, and I had not started medication, I had a nurse who would walk right into my small office (as she should) to talk about anything or everything. I had to just put it out there—if I hold up my hand in a “stop” sign to mean please, for both our sakes, let’s just step into the hall! I did not want to wallow in shame, or to watch her try to ignore what was not avoidable (her faces were hilarious, but I really couldn’t enjoy them)! Sometimes we laughed, but it really helped me to have a plan.
I’ve heard that flight attendants use the term “crop dusting,” or pretending to do an aisle sweep when they need to pass gas. This may be another way to try and cope. If I worked in a small office, even now, I might try to sit in a desk or cubical away from others or place a small fan underneath my desk and set it on a low setting at all times, just in case. It is an easy excuse: “I just feel a little hot.”
How Gas and Odor Affect Each of Us Differently
To understand what methods of gas control can help, we first need to understand a bit about what causes gas and odor. I also want to define some words so that I don’t have to write “smelly farts” 15 more times!
When we say “gas,” many people think we are also talking about burps, or feeling bloated. From here on out, we will only use the word gas or “flatus” to refer to what comes out of your butt (not much better, but we’ll keep trying). We will use the word “odor” or “malodorous” to class it up a bit from the word “smelly.” We will also go ahead and use the word poop instead of stool, because I feel like it and there’s a limit on how classy I can try to get. The term “altered bowel habits” is also used in published papers if you are Googling this for more information and want your search history to look fancy.
Recently, through social media, I have seen questions about gas odor more often. And like everything on the internet, too many “answers” are oversimplified, selling something or just providing false information altogether! Truthfully, the internet is not so much wrong as it is incomplete.
What works for one person may be right for them, but not for everybody. Some people are so invested in their solution that they blame you if that solution doesn’t work the same for you, and they become upset. My advice is to ignore advice from anyone if it doesn’t work for you.
Myths are created when people want to make sense of something, but don’t really have direct evidence to help. Avoid trying to have the perfect explanation! If something works for you, we can honor that, but “why” it works requires actual study.
What to Expect after Surgery When Everyone Has a Different Experience
In terms of post-bariatric surgery expectations:
- Some patients have no problems.
- Many have problems with odor a couple times each week.
- Many patients have loose poop once or twice a month (not everyone feels the same about this, and not every bowel movement has to be perfect).
- Every fart is going to have some odor (except those from unicorns).
Many people notice a difference with gas and odor with just the passage of time. The bowels do adapt to new changes in physiology, but it is often after months or years, and cannot really be altered or hurried. In my experience with patients in my practice, what they notice the most is the noise of gas moving through their system. During the first year after my sleeve gastrectomy, it would wake me up! It was like there was a chihuahua growling somewhere under the sheets, and our Corgi dog in the corner was not amused!
Bloating is usually a very different issue. If you have new problems with bloating several months or years after surgery, consider getting evaluated for reflux in your esophagus or for gallbladder disease. If you had Roux-en-Y gastric bypass surgery, you might need to be checked for a bowel obstruction or an internal hernia. You can address this issue with your primary healthcare provider first, but you will likely need to be examined by your surgeon if the problem is severe or does not go away easily. Don’t be afraid to see your surgeon, especially after gastric bypass surgery.
The Science of Gas and Odor
STINK! What is it? Let’s break it down:
- Sulfur-containing gasses are a side effect of the metabolism (life process) of bacteria in your colon (large intestine).
- Other gasses (nitrogen from swallowed air, carbon dioxide) are odorless.
- Not every bacterium in your gut creates these gasses, and the bacteria that seem to make the most gasses are “feeding” on non-digestible carbohydrates like starch or sometimes lactose.
It is important to know that the majority of the bacteria in our colon are helpful to us, so we do not just want to kill them off. Antibiotics are absolutely not the answer for the average person and should only be considered in cases of non-beneficial infections that usually involve irritation of the colon (colitis or enteritis) or are related to recovery after large antibiotic effects from other treatments (overgrowth of an “infectious” strain of bacteria).
You should always be under the care of a specialist in gut (gastroenterologist) or infectious disease for any prescription medication treatment. You should also expect to have specific studies of your poop performed and likely need a colonoscopy. Do you want me to talk about stool transplants here? No, I didn’t think so. But it really is a thing and has saved many lives.
There are a large number of studies on the gut “microbiome,” or the thousands of different types of bacteria and viruses that live in our colon, but research is still ongoing and primarily focused on describing and tracking cases. To date, there has been very little formal study of odor in people, particularly in practical day- to-day terms.
Probiotics have not been studied for gas odor, but they are thought to be occasionally useful in renewing a healthy bacteria population in people who have been on antibiotics and have had their “normal” population altered. I want to stress that hype to sell these products is rampant. Promises and fuzzy, warm ads about probiotics do not mean you need to empty your wallet!
Your body is a pretty good self-regulating system, and there is no place for “detoxifying” or trying other holistic or natural methods, especially ones that are mainly discussed on the internet. As always, before you try any new treatment, discuss it with your healthcare provider or specialist.
Studies about gas and poop odor after bariatric surgery are all based on “after the fact” questionnaires completed by patients. No other measures of gas or smell have been used. This information is rather weak because it is not being asked in real- time. Unfortunately, research costs a lot of money, so studies like ours have to be thrifty and use fairly small groups and non- expensive, non-invasive tools. We can hope that future research may gather better information by using text messages to allow for more real-time data, or even have a gas sensor for patients. But this is not an area that professors are fighting over.
Can Medication Help?
Right now, the only medication being studied to reduce the odor of farts is Bismuth Subgallate (available in the U.S. as Devrom) and it can be bought without prescription over the counter or online. To give you full disclosure: I take this every single day, and many of my patients do as well.
Our research group performed one of the two studies in the scientific literature for Bismuth Subgallate in patients after bariatric surgery (we specifically studied duodenal switch surgery patients). Both studies confirmed that there is less reported odor and improved quality of life on a validated scientific scale.
Bismuth Subgallate was FDA-approved without a prescription decades ago to reduce odor in patients who had an “ostomy” (bowel emptying into a bag on the abdominal wall—either temporary or permanent). This medication is believed to directly change the bacteria that makes the sulfur-containing gasses. It has only been reported to cause a problem when taken in doses far beyond the recommended dose. Please, don’t do that with ANY medication!
Everyday Changes that Can Offer Help
Changing the type of foods you eat has made a significant difference for some patients when it comes to gas and odor, but you will need to experiment to find what works best for you.
The best thing you can do to avoid odor is to avoid feeding the stinky bacteria too much. Simply put, you can eliminate certain carbohydrates from entering your colon by not consuming them.
The science of carbohydrates in your gut explained:
The science of “sugars” is a bit hard to explain. When we think of “sugar,” most people think of the white sweet stuff in “naughty” foods that we try to avoid to keep weight off. This type of sugar is actually not the problem, because we absorb all of that sugar before it gets to the colon.
Indigestible Starch: The “sugars” or carbohydrates that bacteria in your gut feed from are the ones we can’t absorb. This sugar (indigestible starch) passes into the colon and feeds the bacteria. Indigestible starches are those found in beans and many vegetables like cabbage, peppers, onions and broccoli. These starches are broken down into simple sugars that hang around in the colon, where we can’t absorb them. So our gut bacteria are having a feast! Imagine this like Legos blocks that are glued together. The glue is only dissolved by special tools that only bacteria have.
Lactose: Lactose is the sugar found in milk products. People who have lactose intolerance do not have enough of the enzymes to break up the “Lego chain” type of sugar that cows make (lactose). When lactose enters their colon, it gets broken up and used in a bad way! Many people with lactose intolerance can digest a little at a time, or can handle some yogurts, as the lactose in some yogurt is partially “pre-digested.”
Fructose: Fructose is the sugar naturally found in fruits, some vegetables and honey. Fructose may behave like lactose for some people, but we really don’t have much information. I would not fault you for thinking about it, but people are pretty good at breaking down and digesting fructose. If fructose digestion issues are related to “dumping,” or overwhelming the system, then fructose could easily play more of a role in gas buildup. Timing meals differently or eating more slowly can help some people have less gas. Liquids can be washed down more quickly and may cause problems if there is a lot of sugar—also known as “late dumping” which causes gas and diarrhea more than 30 minutes after eating. As a reminder, early dumping is the effect of fast absorption of sugar, leading to wild ups and downs in blood sugar and insulin which can cause wooziness, lightheadedness, sweats or low blood pressure.
Fizzy drinks with carbonation are mostly absorbed in the gut and we actually breathe out the CO2! Carbonated beverages certainly can make you burp, but they rarely contribute to the amount of farting you do.
On the other hand, when people suffer from heartburn and acid reflux, many people are “air swallowers” when they seek to soothe the pain by chewing gum or trying to force things back down by swallowing saliva (and air). In this situation, controlling heartburn (reflux control from acid blockers, Tums, carafate, and digestive aids like apple cider vinegar) may help reduce the amount of gas down below. This happens because nitrogen is the most abundant gas in the atmosphere and can’t be absorbed, so it travels all the way through. It is odorless, but definitely not silent! Even odorless gas is going to smell some. Still, these are not the patients who tell me that their gas “can peel the paint off the walls and make you cry.”
Other Thoughts for Gas Control:
- Some people may respond well to reduced stress (doesn’t everyone)!
- Some people may respond better to a more forgiving work environment, away from the cube farm.
- Sorbitol sugar-free hard candies can be a problem if you eat more than five to six servings in a day (Sorbitol is totally non- digestible by humans).
- Some people learn over time what are their triggers are and how to avoid them when they know others will be around them.
- Some just feel better knowing they are not alone.
Finally, there are probably a few other tricks and tips we have never heard of before. Please feel free to share them with us!
For additional reading, you can see the article I wrote in 2010 for this same magazine: “Pull My Finger, a Mostly Polite look at Intestinal Gas for Weight Loss Surgery Patients.” It can be found online in the Article Library here.
About the Authors:
Dr. Medlin is the drafting author of this article and takes responsibility for the use of “I” (and maybe credit for making this subject more tolerable), but Dr. Zaveri and Dr. Surve are responsible for the research, editing and any take-away information you may have gotten from this article (and deserve many thanks).
Walter Medlin, MD, FACS, is a bariatric surgeon in Utah and sleeve gastrectomy patient now 10 years post-op. He is a member of the Obesity Action Coalition (OAC) National Board of Directors, tweets from @Bonuslife and runs a personal blog at BonusLife.com.
Hinali Zaveri, MD, has extensive experience in the field of obesity as an active researcher. She is a Bariatric Research Specialist at Bariatric Medicine Institute where she conducts research on various surgical treatments for severe obesity and their beneficial effects on obesity comorbidities. She is an active member of the American Society of Metabolic and Bariatric Surgery (ASMBS) and International federation for the surgery of Obesity and Metabolic Disorders (IFSO).
Amit K. Surve, MD, has been an active researcher in the field of obesity since 2012. Dr. Surve had a major research interest in problems related to obesity, and the various surgical techniques for the surgical treatment of severe obesity and their beneficial effects on obesity comorbidities. Dr. Surve is currently the Editor-in-Chief of the ‘Journal of Obesity Management’ and the ‘Journal of Surgery.’
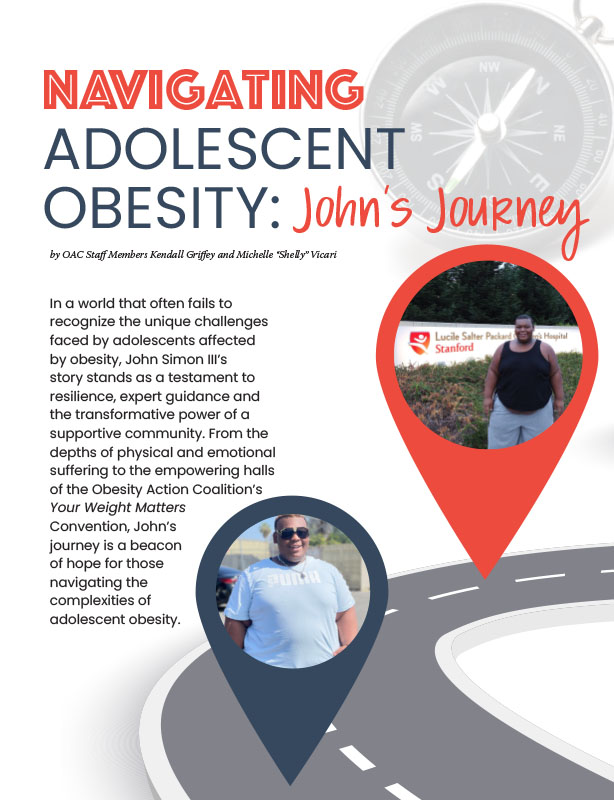
by OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read ArticlePost-operative addiction is often overly simplified as transfer addiction or cross-addiction, assuming individuals “trade” compulsive eating for…
View Video