Obesity and its Treatments: An Overview

by Lisa Saf Koche, MD
Fall 2005
By now I am sure everyone is tired of hearing the statistics; Americans are affected by obesity and the common diseases associated with obesity are increasing at rapid rates.
It is estimated that 64 percent of Americans have excess weight or obesity (those with a body mass index greater than 25). The costs associated with obesity are also mind boggling (approximately $117 billion in 2000) and continually on the rise. With all of this research and information, why are we not able to make a significant change in our approach and to treating obesity?
The answer lies in the fact that obesity is one of the most complex and confusing problems in medicine today. The etiology of obesity includes multiple factors that need to be addressed in order to achieve any significant and sustained weight-loss. In addition, physicians have minimal, or no, training in the management of obesity and often lack the time or interest to properly treat these complex patients. The goal of this article is to provide a broad overview for patients to understand their treatment options.
Measuring Obesity
The initial step in any approach to obesity treatment is the assessment. All patients should be aware of their body mass index (BMI), which is a simple formula using height and weight to determine the level of obesity.
Patients should also have a waist circumference assessment because it enables physicians to estimate the amount of abdominal adiposity, which is an independent risk factor for disease. Patients with an increased waist circumference (greater than 35 inches in women or greater than 40 in men) have higher chances of developing diabetes, fatty liver disease, dyslipidemia, sleep apnea and cardiovascular disease.
Additionally there are more specialized tests typically found only in a bariatrician’s (physicians with specialty training in weight-loss treatment) office such as machines that assess metabolism by oxygen consumption and estimate lean body mass by bioimpedance.
Determining a Patient’s Readiness
After the initial diagnosis of obesity is made, the physician and patient should determine whether, and the extent to which, the patient is prepared and/or ready to lose weight. Bariatricians and their patients typically discuss the risks of obesity and the potential benefits of weight-loss; evaluate previous attempts, successes and failures; and most importantly, rule out any significant depression or depressive symptoms as a casual factor. In the latter regard, depression is very often associated with binge eating disorder or other forms of emotional eating and is a significant barrier to any long term success.
Modifying Your Diet
The second phase in the treatment of obesity involves a discussion of dietary options. A good general rule is to get the patient to decrease their current oral intake by 500-1000 calories per day, which translates into a one or two pound weight-loss per week. The typical caloric intake recommendation is 1000-1200 for women and 1200-1600 for men. Of particular significance, it is unsafe to fall below 800 calories per day.
As everyone is well aware, because of substantial media coverage, the choices of diets is astonishing. In general, a chronic dieter (the classic “yo-yo dieter”) knows more about the different fad diets than most physicians. Fad diets have ranged from the grapefruit to cabbage soup, to the most recent pita pocket diet. Each of these diets claim to be the next answer to long term success with weight-loss.
Perhaps the biggest and most recent craze, the “low carb” diet, is based on the fact that patients are more satiated and seem to lose more weight (at least initially) when diet plans such as Atkins and South Beach are closely followed. A collateral benefit of these diets may be that less processed food is eaten and blood glucose levels tend to stay in the normal range.
The most important and basic principle universal to all diets is that intake greater than output leads to weight gain. For this reason, I recommend portion control, avoidance of all processed foods (stick to the all natural vegetables, lean protein and fruit), consuming some good fat (olive oil, nuts, etc.) and eating small frequent meals. Patients with a higher BMI (greater than 30) may want to consider one of the very low calorie plans (such as Medifast) but should only do so under the guidance and supervision of a properly trained physician (preferably a bariatrician).
Behavior Therapy
It became very clear to me when I started to treat obesity that behavioral therapy is, not surprisingly, a huge key to long term success. There are so many emotional ties to food in that food is cheap, legal and always around when you “need it.” People eat in celebration, sadness, stress, boredom and sometimes (but not often) even when they are hungry.
Patients need to evaluate how much emotional eating exists in their day-to-day life and learn to control it in order to succeed. The quickest tool that is easy (and free) is self-monitoring. For this purpose, I recommend that patients keep a journal with every oral intake documented (be certain to carry the journal at all times, as 30 percent of calories are forgotten if recorded at the end of the day). The patient should also write down his/her mood at the time so that the reason for eating can eventually be shifted to hunger and meal times.
Often the “yo-yo dieter” will have issues such as binge eating, night eating syndrome (when 70 percent or more of the daily calories are consumed after 7 p.m.) or untreated depression. These conditions need more aggressive psychotherapy and treatment prior to attempting any aggressive weight-loss program.
Exercise
Additionally, most patients will not succeed without incorporating exercise into their daily routine. Studies have shown that patients who lose weight become more efficient at any activity. This means if you have lost any significant weight, the energy you burn walking to the mailbox will essentially be cut in half. The body adopts a “starvation” mentality and conserves energy. Therefore, you will have to make two trips to the mailbox in order to burn the same number of calories that you spent before losing weight. This explains why exercise is such a critical part of long term weight maintenance.
Many times patients just need some guidelines on what exercises they should be doing. Often it is a scheduling issue. I tell my patients that exercise should be treated as if it is one of their most important meetings or clients for the day. Many of my corporate patients actually schedule their activity time on their calendar to be sure not to miss a workout.
Treating Obesity Using Medications and Supplements
The medical approach to obesity treatment is complex. The initial evaluation needs to include testing to rule out a medical reason for the weight issue. Hormones such as cortisol and thyroid disorders may be culprits. Patients also need to be stable enough to handle a weight-loss plan (i.e. without active coronary artery disease or going through cancer therapy).
Unfortunately there are only a few weight-loss medications approved by the Food and Drug Administration (FDA). Sibutramine, Xenical and the anorexant class, such as Phentermine or Phendimetrazine, are the most commonly prescribed medications. A new medicine, Rimonabant, will likely be available for prescribing sometime after the first of the year. Rimonabant is generally safe for all patients and is said to help achieve a 20 pound weight-loss in one year.
There are also many nutritional supplements that have been advertised as treatment options for weight-loss, such as CLA and L-Carnitine, but these supplements generally lack substantial evidence supporting their efficacy.
Treating Morbid Obesity
Unfortunately, medical treatment of severe obesity using medications and supplements is weak at best (four to eight percent decrease in body weight typically seen with the above mentioned modalities). Therefore, for patients with a BMI greater than 40, bariatric surgery should be considered as the best chance at long term significant weight-loss (up to 65-75 percent decrease of excess body weight).
The most common procedure is the Roux-en-Y gastric bypass, where a portion of the small bowel is bypassed promoting weight-loss via restrictive (a small pouch size) and malabsorptive means.
The Lap-Band ® procedure is a less invasive option now being commonly performed with good results. There are also some endoscopic procedures (through the mouth) being developed that may soon become an additional, less invasive, choice.
The Results of Treating Obesity
The great news about the treatment of obesity (and why those of us that choose this field love our jobs) is that most of the significant associated co-morbidities seen with obesity are resolved with weight-loss. Weight-loss can lower the mortality rate by up to 24 percent. Even losing 10 percent of your total body weight can significantly improve blood pressure, diabetic control, lipids and arthritis. Many people are also able to get off some, or even all, of their medications. Patients with diabetes or metabolic syndrome can see 75-90 percent improvement rates after gastric bypass surgery.
Therefore, patients and physicians need to approach weight-loss as a chronic disease with a focused treatment plan, which includes a team of healthcare providers. The team should include dietitians, psychologists and exercise specialists, in addition to the medical providers.
With a focused team approach, patients will have all the tools they need to not only succeed in their weight-loss attempts, but to achieve long term maintenance.
About the Author:
Lisa Saff Koche, MD, is the Medical Director for Spectra Healthcare and an Associate Clinical Professor at the University of South Florida in Tampa. Dr. Koche has practiced in obesity for seven years with aggressive medical management as well as complete medical support for bariatric surgery patients.
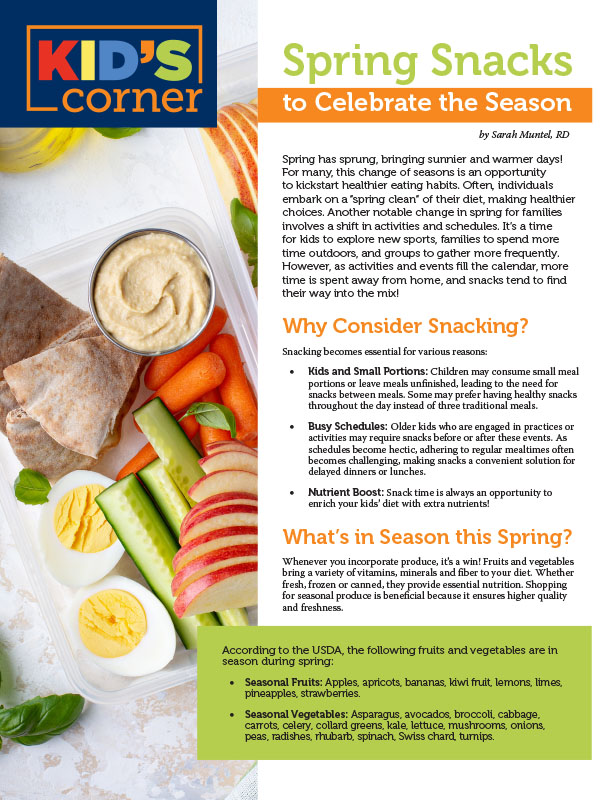
by Sarah Muntel, RD Spring 2024 Spring has sprung, bringing sunnier and warmer days! For many, this…
Read Articleby Yelena Kibasova Spring 2024 The fitness world is evolving, with new trends and innovations that promise…
Read Articleby Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read Article