I need a revision to my bariatric surgery. Will my insurance cover it?

By Gary Viscio, Esq.
Fall 2007
The weight-loss surgery field experienced exponential growth throughout the past four years. As a result, I find myself being asked more and more questions regarding post-operative surgery. Be it plastic surgery, or a revision, the sheer numbers of post-op patients is increasing the demand for these two types of post-op procedures.
In this article, we’ll talk solely about revisions. And that word, revision, gives rise to a number of included terms such as failed surgery, non-compliance, and revision to a new procedure.
Revision, defined, is to change or modify (for our purposes, it is to change or modify a prior bariatric surgery). There are several areas where revisions can arise. A patient will be dealing with either a revision of a failed bariatric procedure or a revision to a new type of procedure not approved or even in existence at the time of the original surgery.
Will My Insurance Provider Cover a Revision?
This is a simple question, but a not so simple response. As we all know, insurance companies seem to make decisions by throwing darts at a dartboard. So it’s only natural to assume that a provider will have different responses for different individuals from different states.
To begin, a request for a revision based upon a failed prior bariatric surgery is going to immediately invoke a response from most insurance providers questioning whether the prior surgery actually failed, or the patient was simply not compliant with the requirements of the first surgery. In other words, eating past the pouch or band.
A revision from a prior procedure to a new type of procedure is going to receive similar questions along with the additional question of why the patient is seeking to change from a Roux-en-Y to gastric banding or duodenal switch.
Before you make this type of request, it is imperative that you and your surgeon are on the same page. He or she should be aware of the exact need for the surgery, as well as your compliance issues during the original procedure. Never wait for the insurance company to ask the question. Answer it when your surgeon submits the request for authorization.
If the pouch stretched, staple line failed, band slipped or bypass simply hasn’t worked, you must have the pre-op testing to prove these allegations. Whether an MRI, CT scan or endoscopy, you should have the results before you apply for certification. Likewise, you should provide your surgeon with a general description of your compliance throughout the years, consisting of a diet and exercise history.
Chances are your body mass index (BMI) has been low at times and you no longer have any significant co-morbidities. In this case, you are going to make sure that the carrier knows that if the revision is not granted, it will only be a short matter of time before your BMI climbs even higher and your co-morbidities return. If your request involves a new type of surgery, perhaps one that didn’t exist when you had your original surgery, make sure the reasons why this surgery is right for you are included in the request for surgery. These pre-emptive strikes just may get you the approval you seek by answering the insurance company’s questions before they’re asked.
I know what you’re thinking. Suppose my insurance company does not or no longer covers bariatric or weight-loss surgery. Well, in that situation you’re going to argue two things. First, that weight-loss surgery should be a covered expense because it is used to treat co-morbidities in addition to obesity, such as diabetes or hypertension. And second, that this is a request to correct a failed procedure that may cause significant problems in the near future and as such it is not for obesity or weight-loss. The latter is a tougher argument, but one that has been made successfully. So remember, like your request for your original surgery, you must document your claims. And, of course, never quit.
About the Author:
Gary Viscio, Esq., is an attorney who specializes in appeals for denials of obesity surgery, reimbursement and coverage, as well as obesity discrimination. In July 2003, he underwent weight-loss surgery and to date has lost more than 160 pounds. He is a member of the Obesity Action Coalition, ObesityHelp Advisory Panel and the Board of Directors of the National Spinal Cord Injury Association. He has handled insurance litigation matters for nearly 15 years.
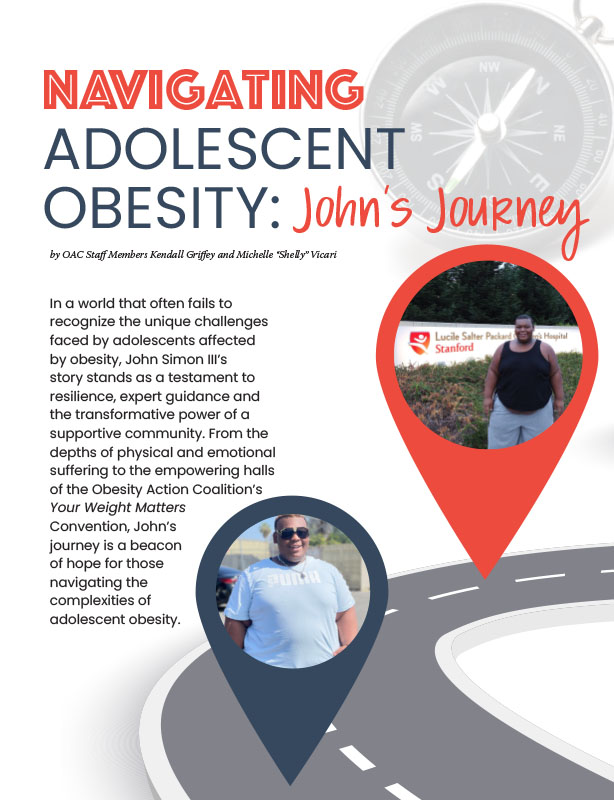
by OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read ArticlePost-operative addiction is often overly simplified as transfer addiction or cross-addiction, assuming individuals “trade” compulsive eating for…
View Video