Dear Doctor: What Can I Do to Treat my GERD?


Answer provided by Gary Reiss, MD
Winter 2016
“As I work to combat my weight gain, I notice myself experiencing more acid reflux-like symptoms. What is this, and is there anything I can do to alleviate it?”
Do you experience chronic heartburn? If so, you could be affected by gastroesophageal reflux disease (GERD). Many individuals with excess weight may be at risk for GERD. In fact, GERD affects roughly 60-70 percent of the population with severe obesity, versus 10-20 percent of the average population.
There are a few reasons for the difference. For some individuals, it is believed that excess weight may press on the stomach, forcing its contents back up into the throat. Overeating may also increase the incidence of reflux, as an over-full stomach stretches the muscles at the top of the stomach, which are designed to keep stomach contents out of the throat.
In patients who have had bariatric surgery, the procedure and resulting weight-loss may resolve GERD symptoms, but for others, GERD continues even after a successful amount of weight is lost following surgery.
GERD occurs when the sphincter muscle between the throat and the stomach allows contents from the stomach to reflux back up into the throat. This continual “wash” of acid, bile and other contents irritates the lining of the throat, which may lead to a condition known as Barrett’s Esophagus, a pre-cancerous condition.
If ignored for too long, this chronic condition may result in throat cancer, which, according to the National Cancer Institute, is the fastest-growing cancer in the United States.
What You Can Do about Your GERD
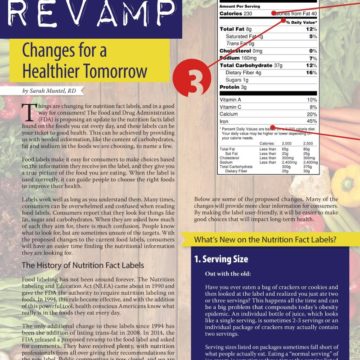
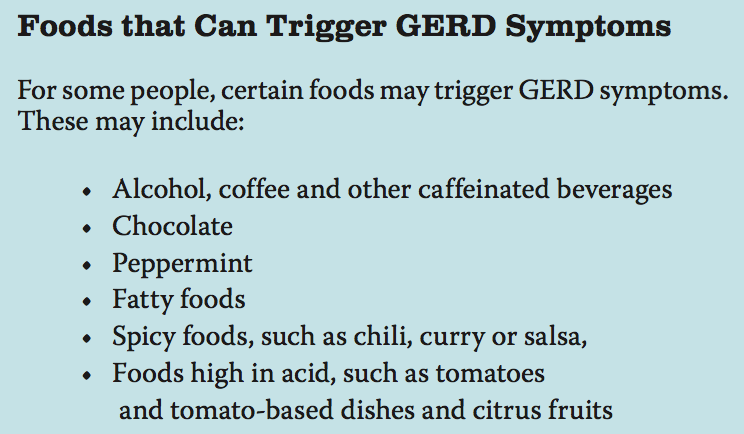
The first strategy for addressing GERD symptoms is lifestyle changes. Doctors recommend eating more frequent and smaller meals, and not eating for at least two to three hours before bed. Some patients find relief from nighttime symptoms by elevating the head of their bed 4-6 inches, either with additional pillows, or raising the end of the bed on blocks.
When Lifestyle Changes Don’t Work
Treatments for GERD begin with the least invasive options and later progress to surgery, such as:
1. Medications
2. Non-Surgical Endoscopic Treatment
3. Anti-Reflux Surgery
If lifestyle changes are ineffective, the next line of treatment is medications, generally proton pump inhibitors (PPIs), which are designed to reduce acid production. However, 30 – 40 percent of patients still have symptoms despite the use of medication.
For these patients, a non-surgical endoscopic treatment called “Stretta” may be a good treatment option. This therapy uses radiofrequency (RF) energy to apply low levels of heat to the muscle that is in between the stomach and the esophagus (the tube leading into the stomach). This improves the structure of the muscle, and helps prevent stomach contents from refluxing up into the throat. The procedure is performed through the mouth, on an outpatient basis, usually under conscious sedation. It is safe and proven to be durable; 10-year studies have shown it to be effective a decade after it is performed.
For some patients, doctors may recommend an anti- reflux surgery called a laparoscopic fundoplication. This procedure reinforces the barrier between the stomach and the esophagus by wrapping the stomach around the lower part of the esophagus. This procedure is generally reserved for patients who have not responded to other forms of treatment.
Special Considerations for GERD in Patients with Obesity
Patients with excess weight have more to think about when considering treatment options for their GERD symptoms:
- Vitamin deficiencies and drug interactions may create problems for patients with obesity who have been prescribed PPIs, especially large doses, and especially when the patient still has chronic symptoms despite the medications prescribed.
- Patients with excess weight may not be good candidates for anti-reflux surgery, due to the historically high failure rate of this procedure in patients with obesity.
- Patients who have undergone bariatric surgery are not candidates for anti-reflux surgery due to their altered anatomy.
- For gastric sleeve patients with chronic GERD that is not responding to medication, one option may be a surgical conversion from sleeve to roux-en-y gastric bypass. But for patients who have had successful sleeve procedures, this may not be a preferable choice.
- Endoscopic treatment may be an ideal option in patients with obesity and patients who have chronic GERD after bariatric surgery, because it is non-surgical, it is performed through the mouth and it doesn’t alter or interfere with the anatomy. Additionally, all surgical options are still possible after this therapy.
Talk to Your Doctor about Your GERD
Regardless of your weight or surgical history, if you experience GERD symptoms, it is important to speak to your doctor. Generally, most doctors will conduct an upper endoscopy to better evaluate a patient’s condition. This is usually done under conscious sedation, and involves inserting a catheter (a thin medical tube) with a camera attached down the throat. This allows the doctor to “see” the tissue in the throat and to evaluate the muscle at the top of the stomach. Other tests may be called for, depending on the actual symptoms and their severity. After evaluating the patient’s condition, the doctor will discuss options for treatment.
The most important thing patients should know about GERD is that treatment options are available, no matter your BMI or your bariatric surgery history. GERD is a serious health condition and should not be ignored.
About the Author:
Gary Reiss, MD, is a gastroenterologist at the Louisiana State University Health Sciences Center in New Orleans. Dr. Reiss received his medical degree from Louisiana State University in New Orleans in 2002 after graduating from Stanford University. In addition to standard endoscopic procedures, Dr. Reiss performs HALO ablation of Barrett’s esophagus, hemorrhoidal treatment, liver biopsy and Bravo acid reflux testing. Dr. Reiss practices at the Marrero office of Metropolitan Gastroenterology Associates, where he has been practicing since 2008. He is board certified in gastroenterology, and has been published in a variety of professional journals. He has been recognized as a “Best Doctors” in an issue of New Orleans Magazine.
by Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Articleby Sarah Bramblette, MSHL Summer 2023 In the final months of 2022, I experienced both the worst…
Read Article