Dear Doctor: I’m considering bariatric surgery. What do I need to know?

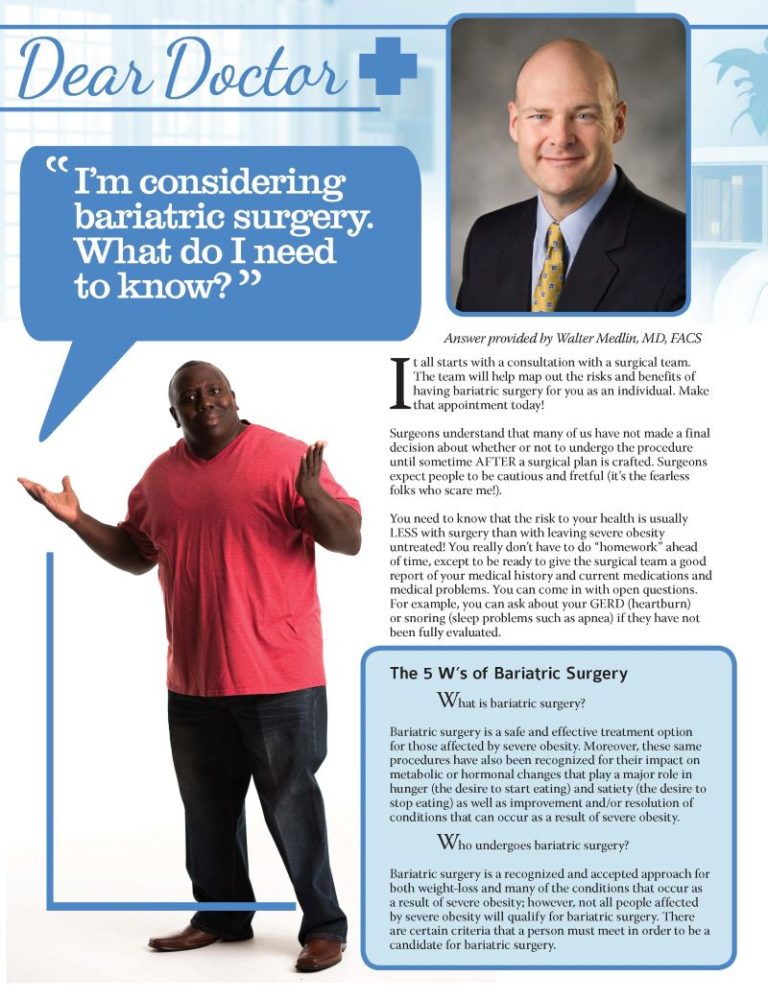
Answer provided by Walter Medlin, MD, FACS
Summer 2016
It all starts with a consultation with a surgical team. The team will help map out the risks and benefits of having bariatric surgery for you as an individual. Make that appointment today!
Surgeons understand that many of us have not made a final decision about whether or not to undergo the procedure until sometime AFTER a surgical plan is crafted. Surgeons expect people to be cautious and fretful (it’s the fearless folks who scare me!).
You need to know that the risk to your health is usually LESS with surgery than with leaving severe obesity untreated! You really don’t have to do “homework” ahead of time, except to be ready to give the surgical team a good report of your medical history and current medications and medical problems. You can come in with open questions. For example, you can ask about your GERD (heartburn) or snoring (sleep problems such as apnea) if they have not been fully evaluated.
The 5 W’s of Bariatric Surgery
What is bariatric surgery?
Bariatric surgery is a safe and effective treatment option for those affected by severe obesity. Moreover, these same procedures have also been recognized for their impact on metabolic or hormonal changes that play a major role in hunger (the desire to start eating) and satiety (the desire to stop eating) as well as improvement and/or resolution of conditions that can occur as a result of severe obesity.
Who undergoes bariatric surgery?
Bariatric surgery is a recognized and accepted approach for both weight-loss and many of the conditions that occur as a result of severe obesity; however, not all people affected by severe obesity will qualify for bariatric surgery. There are certain criteria that a person must meet in order to be a candidate for bariatric surgery.
When is it recommended someone receive bariatric surgery?
The National Institute of Health has identified several criteria for candidacy for bariatric surgery, including:
-
- Body Mass Index (BMI) = a number calculated based on a person’s height and weight:
- BMI >40, Severe obesity (or weighing more than 100 pounds over ideal body weight)
- BMI 35-40 with significant obesity-related conditions (type 2 diabetes, high blood pressure, sleep apnea or high cholesterol)
- No endocrine causes of obesity
- Acceptable operative risk
- Understands surgery and risks
- Absence of drug or alcohol problem
- No uncontrolled psychological conditions
- Failed attempts at medical weight-loss (diets, other weight-loss options)
Consult with your primary care provider (PCP) and insurance provider to see if you are a candidate.
Where is the procedure completed?
The procedure is typically performed at a hospital, and the length of stay varies depending on the procedure chosen.
Why would someone have bariatric surgery?
Within two to three years after the operation, bariatric surgery usually results in a weight-loss of 10 to 35 percent of total body weight, depending on the chosen procedure. Those considering bariatric surgery should talk to their healthcare provider about what their personal expectations should be for loss of excess weight. In addition, co-morbidities, such as diabetes, high blood pressure, sleep apnea and others are often reduced or may go into remission. Most will find they require fewer medicines throughout time and many will discontinue their medicines completely.
“It is a lifelong disease, but we have many good tools to treat it, and many wonderful providers who are available to help!”
You can look into insurance coverage, but do not jump to conclusions until you have had a consultation – there are often options and appeals throughout the process. The resources from the OAC are a great place to gather information for background, but don’t leap to conclusions based on “civilian” articles. Being informed is helpful, but often things need a more complex team approach.
People commonly make assumptions about the limitations of bariatric surgery with age, cancer or surgery history, the ability to exercise, possible food restrictions, the recovery process and family life, and when it’s time to return to work. This is more than I can address here, but be assured – your team will take the time and you can always keep asking questions!
In terms of your health, remember that the goal of bariatric surgery is to help your OVERALL quality of life, not just to help you lose weight. This means good care and evaluation of various health areas, such as stress and mental health issues, heart and lung health, and low vitamin or iron levels (most are low on Vitamin D).
Many of these “hurdles” are not meant to be difficult, but making the risk as low as possible is not always simple. A friend of mine calls it “getting your ducks in a row” – making sure that you don’t accidentally have some factor working against your best chance for safety and good results – both in the short and long-term.
Most importantly, do not worry about being “rejected” for bariatric surgery. This very rarely occurs for a few patients who are not able to take care of themselves safely or who threaten a caregiver. Most other issues can be modified, even if it takes some extra time. On the other hand, if you need to check out a few different programs to get the right fit, go right ahead! Feeling comfortable with my surgeon was super important to me, and I know a lot of surgeons.
Almost all programs offer lifelong follow-up, but many patients do not see great value after a few years, and they drift away. This is a real mistake – long-term issues can sneak up on all of us! I am now almost eight years out from when I had bariatric surgery and I still see a dietitian yearly and a coach or trainer weekly. Even though I know a lot, an outside perspective and professional support keeps me from falling victim to gaps in my own self-knowledge.
Finally, stay empowered. The disease of obesity makes people feel helpless. It is a lifelong disease, but we have many good tools to treat it and many wonderful providers who are available to help! Stay engaged with your healthcare provider and your surgical team, and be ready to spend some time throughout the rest of your life at least paying attention to healthy habits and managing hunger.
Additional Resources to Learn about Bariatric Surgery:
- Obesity Action Coalition: www.ObesityAction.org
- Obesity Help – www.ObesityHelp.com
- Weight Loss Surgery Foundation of America: www.WLSFA.org
- BariatricPal: www.BariatricPal.com
About the Author:
Walter Medlin, MD, FACS, is a bariatric surgeon in Utah and sleeve gastrectomy patient now seven years post-op. He is a member of the OAC National Board of Directors and tweets @bonuslife.
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
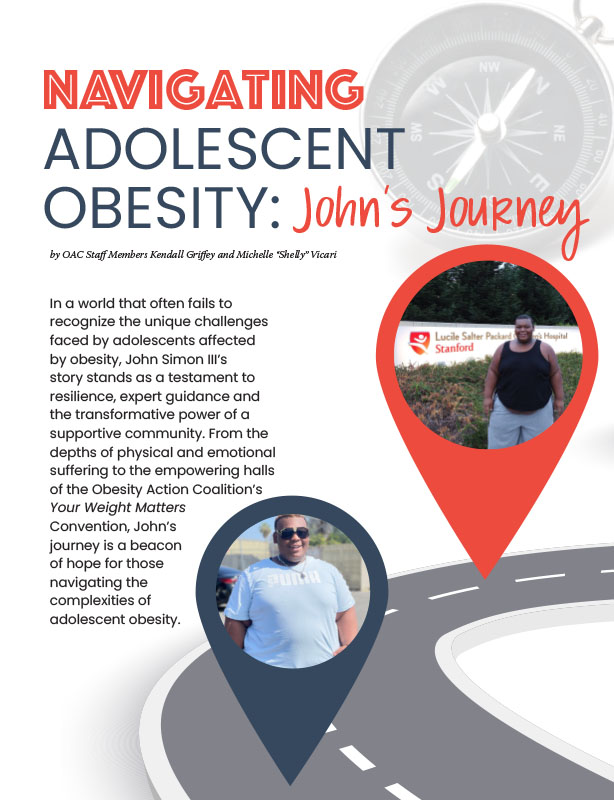
Read Articleby OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Article