Connecting Osteoarthritis and Obesity

by Kirsten Ambrose, MS, CCRC
Summer 2016
Hardly a day goes by without a news story or the latest statistic mentioning the growing obesity epidemic in the United States. Indeed, the number of adults who are affected by obesity has reached 78 million, and no state in the Nation reports fewer than 20 percent of its residents as having obesity.
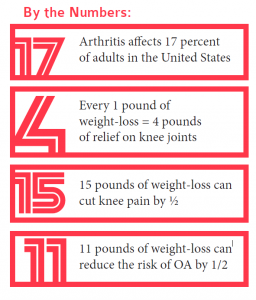
However, many days and even weeks can go by without any news stories or updated statistics on the soaring rate of osteoarthritis (OA). Did you know that OA is the number one cause of disability in the U.S.? Or that it affects nearly 31 million people? Arthritis affects at least 17 percent of adults in every state, with women being more frequently affected than men.
Unfortunately, as childhood obesity rates continue to rise, people are developing OA at younger ages than ever before. Osteoarthritis and obesity are connected — and here’s how.
Osteoarthritis and Obesity: An Unfriendly Connection
It is well known that people with excess weight or obesity have a higher risk of developing other chronic illnesses such as diabetes, heart disease and cancer. They are also at major risk for developing OA.
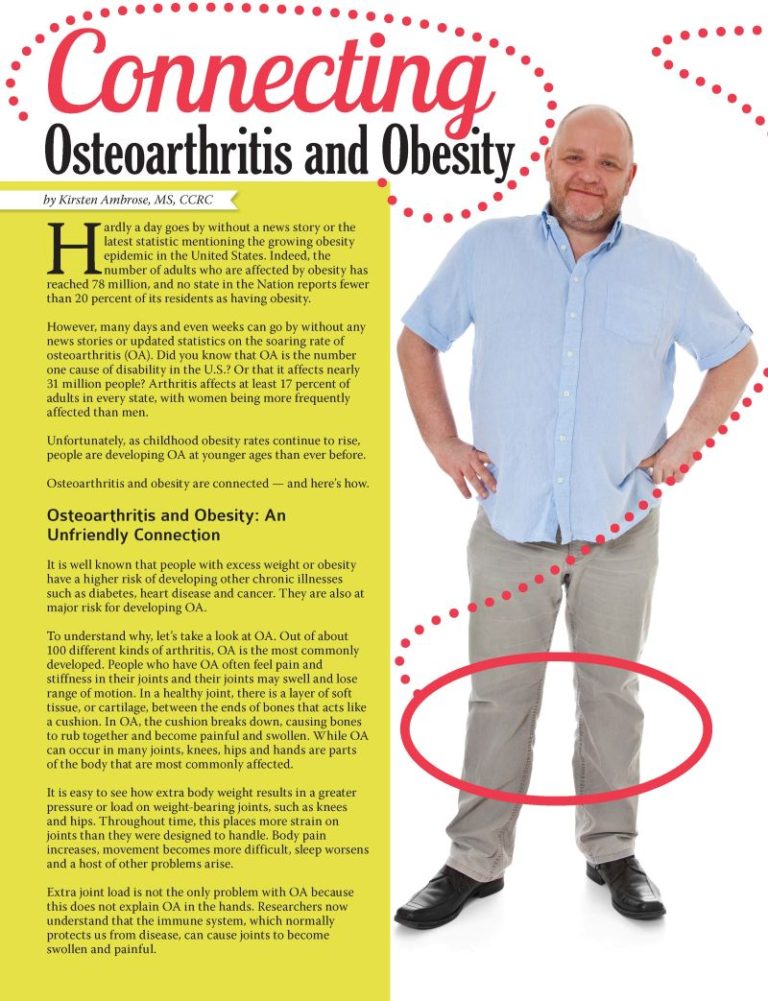
To understand why, let’s take a look at OA. Out of about 100 different kinds of arthritis, OA is the most commonly developed. People who have OA often feel pain and stiffness in their joints and their joints may swell and lose range of motion. In a healthy joint, there is a layer of soft tissue, or cartilage, between the ends of bones that acts like a cushion. In OA, the cushion breaks down, causing bones to rub together and become painful and swollen. While OA can occur in many joints, knees, hips and hands are parts of the body that are most commonly affected.
It is easy to see how extra body weight results in a greater pressure or load on weight-bearing joints, such as knees and hips. Throughout time, this places more strain on joints than they were designed to handle. Body pain increases, movement becomes more difficult, sleep worsens and a host of other problems arise.
Extra joint load is not the only problem with OA because this does not explain OA in the hands. Researchers now understand that the immune system, which normally protects us from disease, can cause joints to become swollen and painful.
For more than 30 percent of Americans who have both arthritis and obesity, the combination results in physical inactivity, followed by additional weight gain and joint strain. For some, this leads to disability and a loss of income, and still more weight gain and joint pain. It can take very little time for a vicious cycle to develop, which results in worsened overall health, poor quality of life, loss of independence and higher healthcare costs for the patient and society in general. This cycle is extremely hard to break, but it can be done.

Osteoarthritis used to be thought of as a disease that happened to older adults. However, as childhood obesity rates have gone up during the last couple of decades, the average age of people experiencing OA has been lowered. We are now seeing adults in their 30s and 40s developing OA due to obesity in their childhood.
When people develop OA earlier in life, they are much more likely to need joint replacements later on. If body weight remains excessive in people who have OA, the affected joint continues to worsen and the potential for joint replacement increases. Joint replacement surgery is expensive and comes with serious risks.
When left unchecked, OA and obesity can wreak havoc on a person’s health, life and well-being. To maintain better health, it’s important to keep joints as healthy as possible for as long as possible to avoid replacement or disability.
“When left unchecked, OA and obesity can wreak havoc on a person’s health, life and well-being. To maintain better health, it’s important to keep joints as healthy as possible for as long as possible to avoid replacement or disability.”
Physical Activity and Weight Management – A Winning Combination
The good news is that simple strategies such as physical activity and weight management can have a significant impact on both OA and obesity. To be clear, “simple” is not the same as “easy” in this case. No doubt, exercising with painful joints can be slow going and, well, painful. The idea of losing a large amount of weight can be overwhelming and downright discouraging.
Simple, in this case, means there is no magic, no trick, no complicated formula and no way around it. Simply taking a small step in the right direction can make a big difference.
Researchers have found that every one pound of weight-loss translates to four pounds of relief on knee joints. Weight-loss of 15 pounds can cut knee pain in half. For people with excess weight who do not yet have OA, an 11-pound weight-loss is enough to reduce the risk of developing knee OA by half.
Researchers have also shown that moderate-intensity, low-impact physical activity such as walking or swimming reduces arthritis pain, and increases the ability to complete daily activities, one’s mood, sleep and quality of life. This level of physical activity does not cause symptoms to worsen or arthritis to become more severe. Physical activity along with a healthy diet also helps people manage weight.
Knowing that physical activity and weight management are important for joint health is one thing. Taking the first step is another thing altogether.
Here are a few keys to success:
- Discuss a plan for weight-loss or physical activity with your doctor or qualified healthcare provider. This person can work with you to tailor a plan to meet your needs and goals to ensure your safety and success.
- With physical activity, everything counts.
The idea is to move more than before. The National Physical Activity Guidelines for Americans give specific recommendations to achieve a certain amount of time and intensity over the course of a week. This is certainly useful for a lot of people. However, for people who are just starting out, who have joint pain, and who are affected by obesity, these guidelines can seem overwhelming. - Set realistic, achievable goals for weight-loss and physical activity.
A good mantra is to “start low and go slow.” Behavior change, and that is what we are talking about, is hard. Make small changes to your diet and activity, and get used to them for six to eight weeks before making more changes. - Take part in enjoyable activities.
Fun, pleasant activities are often the first to go when pain limits movement and daily functioning. Quality of life suffers without joy, regardless of pain. That’s why it’s essential to focus on activities you enjoy. - Find physical activity programs that are local and convenient.
There are many programs that are known to help people with arthritis. A few examples include “Enhance Fitness,” which is offered by many local YMCAs, Zumba classes, Fit and Strong! and the Arthritis Foundation’s Walk With Ease program. Some are offered in group formats, while others can be self directed. The Arthritis Foundation recently launched a Resource Finder to locate programs like these in local communities around the country. You can visit it at www.ResourceFinder.Arthritis.org.
Conclusion:
The combination of OA and obesity have the potential to create significant burdens for patients, their care givers and their community. By learning more and taking action, people with OA can have greater control over their health, and that is always a “step” in the right direction!
The Osteoarthritis Action Alliance (OAAA) is Working Hard to Bring About Change
The OAAA is a coalition of 90 organizations that are concerned with reducing the national impact of OA. A few examples of OAAA members include the Obesity Action Coalition, The Obesity Society, American Physical Therapy Association and the American College of Sports Medicine.
The Alliance is raising awareness about OA and provides educational resources as well as links to community programs that can help people learn about and better manage arthritis. It also promotes strategies such as injury prevention and weight management.
The OAAA proactively reaches out to policymakers at all levels, encouraging them to consider OA in programming and funding decisions. Ultimately, thegoal is to get healthcare systems and providers to improve care for people with this disease.
Anyone may access the many free resources, brochures, and other educational materials available on the OAAA Web site (https://oaaction.unc.edu). Several that were developed jointly with OAC include:
-
- Weight Gain and Joint Pain
- Can My Weight Make My Joint Pain Worse?
- Background Facts on the Vicious Cycle of Obesity, Osteoarthritis (OA), and Disability
About the Author:
Kirsten Ambrose, MS, CCRC, is Program Manager of the OA Action Alliance at Thurston Arthritis Research Center, University of North Carolina. Learn more at oaaction.unc.edu. Ms. Ambrose has a master’s degree in exercise science and is a believer in the benefits of physical activity for absolutely everyone.
by Sarah Ro, MD; and Young Whang, MD, PhD Fall 2023 Mary, a postmenopausal woman with a…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Articleby Sarah Bramblette, MSHL Summer 2023 In the final months of 2022, I experienced both the worst…
Read Article