Pregnancy after Weight-Loss Surgery

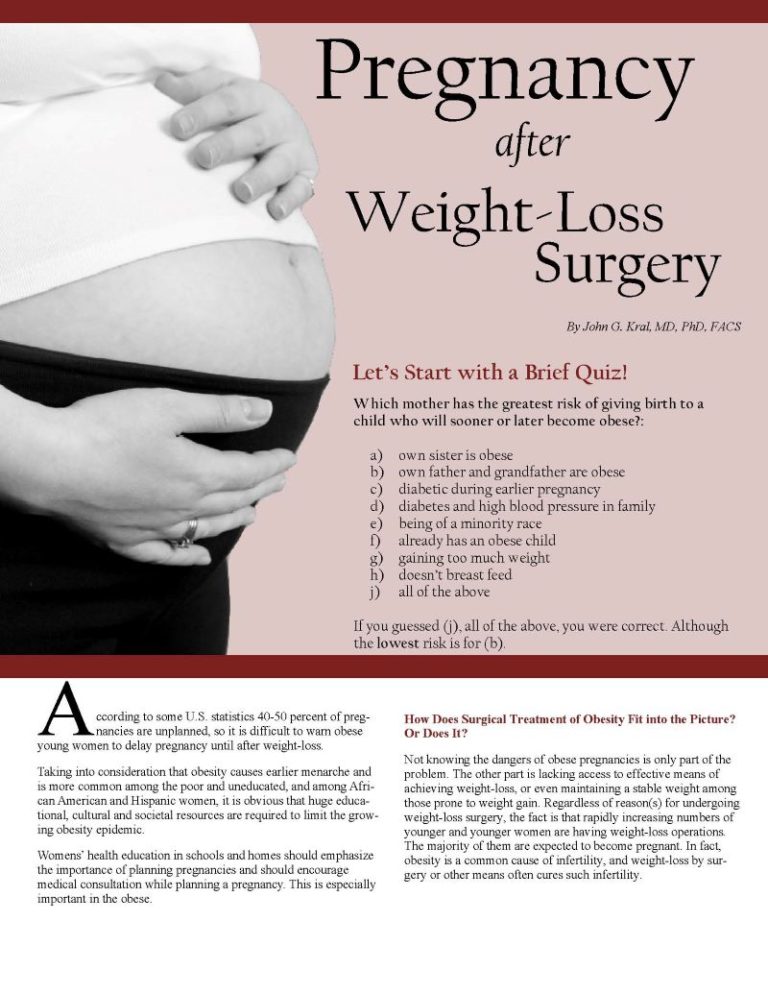
By John G. Kral, MD, PhD, FACS
Spring 2007
According to some U.S. statistics 40-50 percent of pregnancies are unplanned, so it is difficult to warn young women with obesity to delay pregnancy until after weight-loss. Taking into consideration that obesity causes earlier menarche and is more common among the poor and uneducated, and among African American and Hispanic women, it is obvious that huge educational, cultural and societal resources are required to limit the growing obesity epidemic.
Womens’ health education in schools and homes should emphasize the importance of planning pregnancies and should encourage medical consultation while planning a pregnancy. This is especially important in those affected by obesity.
How Does Surgical Treatment of Obesity Fit into the Picture? Or Does It?
Not knowing the dangers of pregnancies with obesity is only part of the problem. The other part is lacking access to effective means of achieving weight-loss, or even maintaining a stable weight among those prone to weight gain. Regardless of reason(s) for undergoing weight-loss surgery, the fact is that rapidly increasing numbers of younger and younger women are having weight-loss operations. The majority of them are expected to become pregnant. In fact, obesity is a common cause of infertility, and weight-loss by surgery or other means often cures such infertility.
What should women with obesity considering surgery, or having undergone weight-loss surgery, know about its effects on pregnancy outcomes?
First, it is important to understand the differences between the two major types of operations. Most operations nowadays are (or should be) performed using a laparoscope and three or four instruments inserted through half-inch cuts in the belly wall, instead of one large cut eight to 12 inches long.
One type of operation is purely “gastric restrictive,” creating a small stomach pouch by placing an adjustable band around the top of the stomach. The inflated band makes a very small opening for the food to pass into the large stomach below the band. This causes small amounts of solid food to stretch the stomach pouch wall creating a sense of fullness as well as slowing the emptying of solid food from the small pouch. Liquids and melting foods (chocolate, cookies, chips) go straight through unless solid food is blocking the opening.
The other type of operation combines restriction (a small pouch) with bypass of more than 95 percent of the stomach and the first portions of the small bowel. The restrictive sense of fullness disappears over the first 10-18 months because the pouch and the opening between the pouch and the small bowel stretch.
The bypass operations work better because the undigested solid food and liquids cause fullness even after the pouch and opening have stretched. Clearly the restrictive action of the operations can cause vomiting, especially if the patient eats quickly and chews poorly. Pills or capsules can similarly cause vomiting if they are sufficiently large.
Weight-loss operations are designed to cause rapid weight-loss which obviously is what the “customer” desires. I’ve already answered the question: “Will weight-loss surgery influence my ability to become pregnant?” But, what about the effects on the pregnancy, the fetus, the delivery and the developing infant on its way into childhood, adolescence and adulthood?
Effects on Pregnancy Outcomes
It is always recommended that young women, who have undergone weight-loss surgery and have the capacity to conceive, should take precautions to prevent pregnancy during the phase of rapid weight-loss, and at least for 18 months to two years after their surgery.
Pregnancy outcomes after all types of weight-loss surgery – even the problematic old intestinal bypass operations and the complex modern aggressive operations with the ability to cause deficiencies and other nutritional problems – are universally safer and better than outcomes of pregnancies with obesity. Even if mothers are still affected by obesity after their surgery, the outcomes are better than if they haven’t had surgery.
Having said this, it is important to recognize that there are risks caused by weight-loss operations if the mother fails to follow recommendations about responding to vomiting, diarrhea or feelings of weakness. Patients must take recommended supplements, and blood levels of critical nutrients must be monitored as part of responsible prenatal care. As is the case for all patients who have had obesity surgery, the rules of eating and vomiting must be followed (please see box at the bottom of this page).
The most recent information about outcomes after obesity surgery suggests that guidelines for “healthy weight gain” should be revised. Commonly, normal-weight women with a body mass index (BMI) of 19.8-26 are recommended to gain 25-35 pounds, while those in the “high range” (BMI of 26.1-29) should have a “recommended target weight gain of at least 15 pounds” according to the Institute of Medicine of the National Academy of Sciences.
The dramatically increasing numbers of women with obesity have provided more statistics on pregnancy weight change in women with severe obesity (BMI greater than 35) allowing the development of new guidelines. Women with severe obesity often lose weight during pregnancy and the outcomes after weight-loss surgery, even during the non-recommended early rapid weight-loss phase, are healthy despite the absence of any weight gain.
Thus, it is important to “spread the word” that women with severe obesity (those with a BMI greater than 35) and those who have undergone weight-loss surgery can actually lose weight with a healthy outcome for the offspring. However, never forget that essential vitamins, minerals and other nutrients must be monitored and supplemented as needed to optimize pregnancy outcomes in those affected by obesity, before and after surgery.
Effects on the Child
Mothers with obesity give birth to small for age or underweight infants more often than lean mothers. After having weight-loss surgery, mothers do not have any increase in the numbers of small offspring compared to when they were affected by obseity. Only recently it has been recognized that small children are “healthy.” In fact, it is dangerous for small (or even premature) infants to gain weight quickly. Rapid weight often leads to childhood obesity. It is important to realize that pregnancies with obesity and early rearing practices can cause many problems. No more, are the old expressions as acceptable: “cute baby fat,” “she’ll grow out of it.” Round pudgy cheeks are not the signs of a “healthy baby.”
Women with obesity do not breast-feed as commonly as non-obesity women. When they do breast-feed, women with obesity do so for a much shorter period of time. Shorter breast-feeding practices are associated with greater post-natal body weight in the mother and increased obesity in the child. Everything must be done to encourage breast-feeding. It is a very healthy and rewarding practice, and it has a role in preventing obesity in the mother and child.
Conclusions
Pregnancies with obesity are dangerous pregnancies.
Pregnancies following weight-loss surgery are safer than pregnancies with obesity for mother and child.
Pregnancies after weight-loss surgery, regardless of weight:
a.) should be prevented during the first 18 months after surgery.
b.) should be monitored for nutrient deficiencies to guide taking supplements.
Recommendations for Pregnant Women who have Undergone Gastric Restrictive Weight-loss Operations
Eating behavior
To reduce the risk of vomiting:
|
|
|
|
|
|
Response to vomiting
If you vomit or regurgitate:
|
|
|
|
|
About the Author:
John G. Kral, MD, PhD, FACS, received his M.A. degree in Psychology in 1961 from the University of Göteborg, Sweden, where he then attended medical school, completed specialty training in surgery and subsequently defended a Ph.D. thesis entitled, Surgical Reduction of Adipose Tissue in 1976. In 1980, Dr. Kral was recruited to St. Luke’s Hospital Center, Columbia University College of Physicians and Surgeons, to develop a program of surgical metabolism and anti-obesity surgery where he investigated eating behavior and continued studies on severe obesity and effects of long-term maintenance of significant weight-loss on body composition after malabsorptive and gastric restrictive operations.
by Kendall Griffey, OAC Communications Manager Spring 2024 We have officially kicked off Your Weight Matters Regional…
Read Articleby OAC Staff Members Kendall Griffey and Michelle “Shelly” Vicari Winter 2024 In a world that often…
Read Articleby Rachel Engelhart, RD; Kelly Donahue, PhD; and Renu Mansukhani, MD Summer 2023 Welcome to the first…
Read Article