Healthcare Reform: How the Legislation Affects You


by Morgan Downey, JD
Spring 2010
Political passions may still be running high, but the healthcare reform legislation has become the law of the land. The Department of Health and Human Services (DHHS) under Secretary Kathleen Sebelius has begun the implementation process. What does it mean for those affected by obesity? It depends on whether you now have health insurance and where you get it.
Changes Taking Place in 2010
Many of the insurance reforms kick in this year. If you do not have health insurance and have had a pre-existing condition for more than six months, you will be able to purchase insurance from a temporary fund. Also, beginning soon insurance companies will be required to keep coverage for children of policy-holders up to age 26.
In addition, health plans must provide, without cost-sharing, preventive services which include intensive behavioral counseling for obesity. Lifetime limits on health insurance will be eliminated and insurers will not be able to rescind coverage except in cases of fraud. Rescinding coverage is where the entire policy is canceled when you get sick. Obesity has been used to justify rescissions. Also, children cannot be denied coverage for pre-existing conditions.
Looking Forward
Starting in 2011, Medicare will pay 100 percent of actual charges for preventive services, including behavioral counseling for obesity. Medicare beneficiaries will also be entitled to a comprehensive health risk assessment and a personalized prevention plan. Incentives will be developed to encourage participation in behavior modification plans. Also, chain restaurants and vending machines will have to disclose calories of each item.
In 2013, the threshold for deducting medical expenses which are not reimbursed rises from 7.5 percent of adjusted gross income to 10 percent. This could have a serious, negative impact on patients who have bariatric surgery and pay out of pocket.
By 2014, state or regional health exchanges will be available. U.S. citizens will be required to have health insurance. If their employer does not provide it, they will be able to purchase coverage in exchanges.
Medicare/Medicaid
While the legislation includes intensive behavioral counseling for obesity in the private insurance market, Medicare and Medicaid, it is less clear on the coverage of bariatric surgery. The current Medicare coverage of surgery is unlikely to change. Medicaid covered benefits have not changed. However, the DHHS will have to define the benefit packages for employers to have a qualified health plan and for the health exchanges. These may or may not include bariatric surgery.
Other Provisions
Other provisions are likely to be important to persons with obesity. Of particular value for persons with morbid obesity, one section provides for the removal of barriers to medical devices for individuals with disabilities. Under this provision, standards will be developed for medical diagnostic equipment used in most medical settings to ensure that the equipment is accessible and usable by individuals of size.
There is one potential loophole which can really hurt persons who have excess weight or obesity. Starting in 2014, employers can institute wellness programs which give some employees a “reward” from 30 percent up to 50 percent of the total cost of their health insurance premium for meeting employer-specified health conditions. This is a big change from current law which only allows “rewards” of up to 20 percent and then only for participating in a wellness program, not meeting a specific outcome, such as a body mass index (BMI) number.
Many employer wellness plans now cover weight management, but their outcomes are no better than other self-help programs. With this new law, employers will have the ability to shift a great deal of their healthcare expenses onto persons who cannot meet artificial and unattainable weight targets.
The legislation also contains many provisions targeting the prevention of obesity, including developing a national strategy, creating healthier school environments and targeting a variety of age levels to increase access to nutrition and physical activity.
Conclusion
As they say, “the devil is in the details,” and that could not be truer than in the wake of healthcare reform. How the regulations are written, what the courts do and how the market responds will determine the eventual value of this legislation.
About the Author:
Morgan Downey, JD, is the former director of both The Obesity Society and the American Obesity Association. He currently consults on obesity policy and publishes the Downey Obesity Report. For a more in-depth analysis of the healthcare bill and to follow the developments of healthcare legislation, please view www.downeyobesityreport.com.
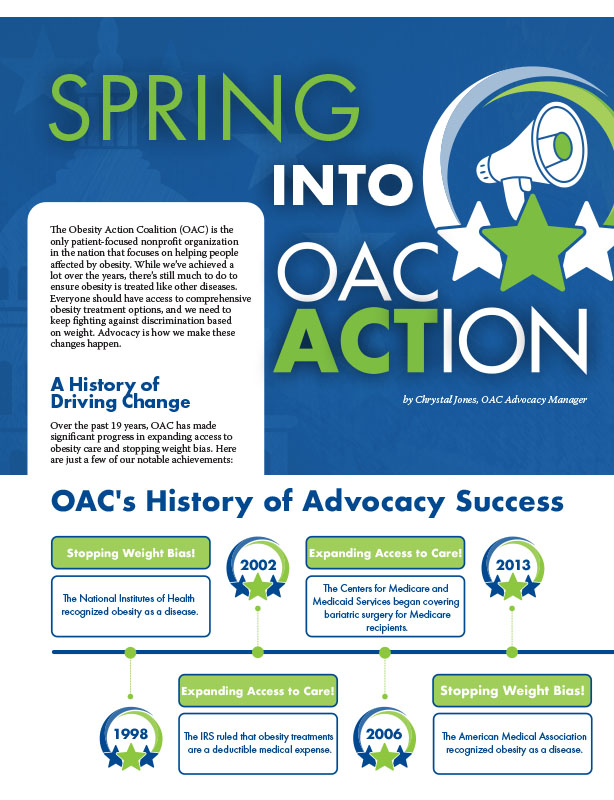
by Chrystal Jones, OAC Advocacy Manager Spring 2024 The Obesity Action Coalition (OAC) is the only patient-focused…
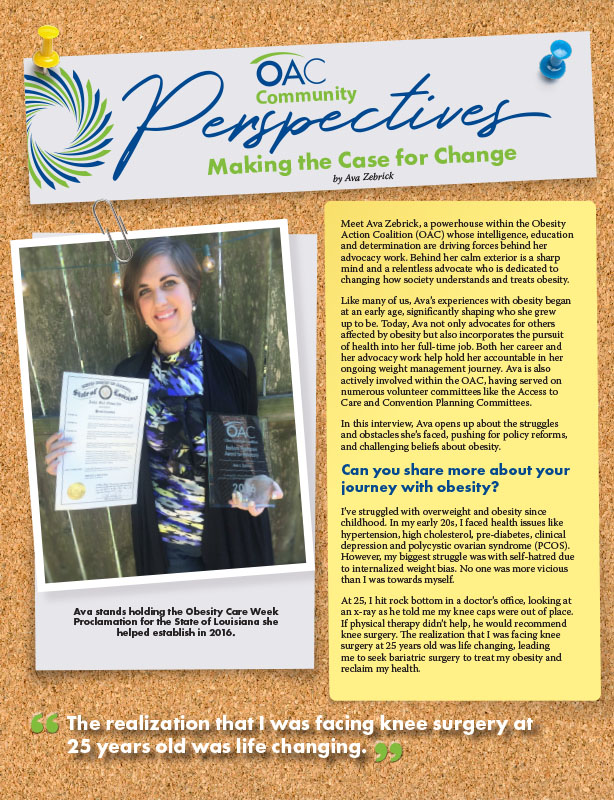
Read Articleby Ava Zebrick Spring 2024 Meet Ava Zebrick, a powerhouse within the Obesity Action Coalition (OAC) whose…
Read ArticleThe OAC is honored to welcome three new members to the OAC National Board of Directors. Jason Krynicki,…
Read Article